Over the past twenty years, advances in translational medicine have resulted in new and exciting treatments in the area of oncology. New modalities have arisen out of the need to address existing limitations in conventional treatments such as chemotherapy and radiotherapy. What started out as an outrageous idea in the 20th century to use potentially dangerous infectious agents such as viruses to kill cancer cells has gradually evolved into a maturing field, which has the promising potential to incorporate conventional and immunological aspects of treatment within a microbial-based system. Finally, in 2006, the introduction of the world’s first approved oncolytic virus by China heralded a milestone in the clinical application of this approach. This article will examine use of oncolytic viruses in cancer treatment with emphasis on its current status and strategies, possible immune mechanism and future considerations.
Over the past twenty years, advances in translational medicine have resulted in new and exciting treatments in the area of oncology. New modalities have arisen out of the need to address existing limitations in conventional treatments such as chemotherapy and radiotherapy. What started out as an outrageous idea in the 20th century to use potentially dangerous infectious agents such as viruses to kill cancer cells has gradually evolved into a maturing field, which has the promising potential to incorporate conventional and immunological aspects of treatment within a microbial-based system. Finally, in 2006, the introduction of the world’s first approved oncolytic virus by China heralded a milestone in the clinical application of this approach. This article will examine use of oncolytic viruses in cancer treatment with emphasis on its current status and strategies, possible immune mechanism and future considerations.
Introduction
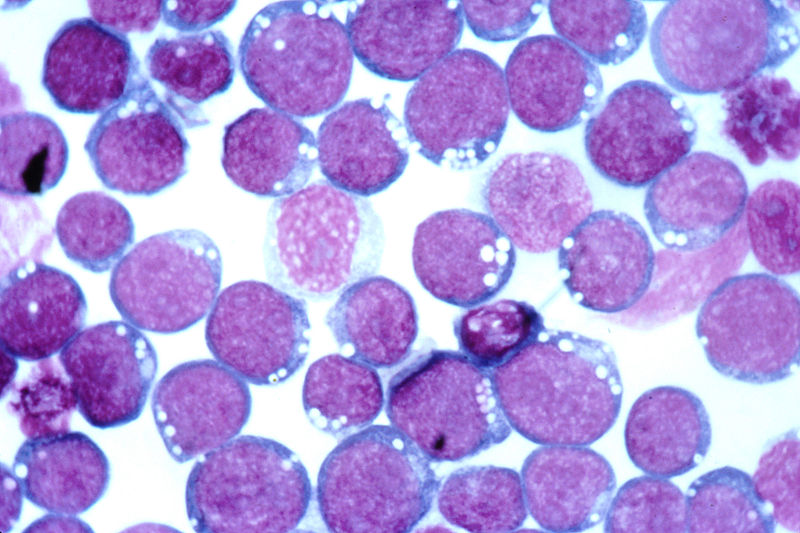
Oncolytic viruses are self-replicating viruses which can target and lyse cancer cells specifically. [1] Since the early 1900s, it was recognised that natural viral infections in cancer patients are sometimes associated with tumour regression. Indeed, case reports noted instances where influenza or measles infections in leukemia patients resulted in remissions. [2] Interest in utilising these ‘cancer-killing’ viruses peaked in the 1950-60s but the rise of chemotherapy and radiotherapy meant that progress in this field stagnated until the 1990s, when genetic engineering and better understanding of viruses and tumours revived the development of oncolytic viruses. [3] A breakthrough in the clinical translation of oncolytic viruses finally came in 2006 with the world’s first approved oncolytic virus- H101 (a genetically modified adenovirus) for head and neck cancers. [4]
Why oncolytic virotherapy?
Conventional treatments such as chemotherapy and radiotherapy have been the cornerstone of oncological management for many years. While we have achieved a considerable amount of success in many cancers, there are often criticisms against conventional treatments in terms of their limitations (e.g. transient effects against metastasis) and flaws (e.g. poor toxicity profile). [5] In recent years, gene therapy and immunotherapy have emerged as alternatives but results have been mixed. In 2002, the development of leukaemia in x-linked severe combined immunodeficiency (X-SCID) patients due to insertional mutagenesishas severely affected public confidence in gene therapy. [6] While immunotherapy remains promising, the current emphasis on specific targeting neglects the ability of tumour cells to mutate and change antigen profiles, resulting in variable clinical outcomes. [7]
In view of these insufficiencies, there has been renewed interest in oncolytic virotherapy, an interesting cross-disciplinary approach to treatment based virology, genetic engineering and immunology. The initial thinking behind this approach was simple- certain viruses exhibit tropism for cancer cells, which either express specific receptors for viral entry or lack anti-viral mechanisms that are normally intact in normal cells. [8] Once viral entry is achieved, replication of viruses continues until cell lysis occurs; allowing their progeny to infect other cancer cells. If viral spread is homogenous, the oncolytic effect can be amplified many times and this effectively destroys the whole tumour. [8] As therapeutic genes encoding pro-apoptotic and immune effectors can be incorporated into the viral genome, an effective anti-tumour response may be initiated and magnified with each replication. [9] The ingenuity of this idea is that it exploits the infectious nature of viruses and uses it as a carrier and amplifier of other therapeutic agents. The latter may be crucial in exploiting synergistic anti-tumour effects between distinct treatment modalities.
Current status of oncolytic virotherapy
A variety of natural occurring and genetically modified viruses have been tested in clinical trials (Table 1).
Natural occurring oncolytic viruses are chosen for their low pathogenicity and inherent specificity for tumour cells. [10] Conversely, genetically modified viruses are those that are modified to promote tumour specificity, for example through use of tumour-specific promoters and gene deletions, or reduce pathogenicity by serial passage through cell culture. [8] Based on clinical data, it has been shown that virotherapy has a favourable toxicity and safety profile as compared to conventional treatment; the most common side effects being fever,flu-like symptoms and safety issues mainly concerning viral shedding and mutation-induced pathogenesis. [1,11] For the latter, dosing limitations and use of pro-drug activating suicide genes have addressed many of these issues. [1,6]
A straightforward dose-response relationship is not often observed as viral replication occurs in a heterogeneous tumour microenvironment and depends on factors such as availability of cell surface receptors and anti-viral responses. [12] Efficacy varies between different viruses but is reasonable at this early stage of development. The clinical trial for H101 reported complete remissions and partial responses in three and eleven out of forty-six patients respectively while another modified adenovirus- ONYX-15 was also used in head and neck cancer trials and achieved tumour growth stabilisation in eight out of twenty-two patients and tumour necrosis in five out of twenty-two patients. [11,13]
It appears that limitations in efficacy were due to certain barriers. Firstly, viruses are not adept at surviving in the circulation. They are subjected to neutralising antibodies, complement and sequestration by the reticuloendothelial system. [8] In some cases, previous viral exposure may result in pre-existing anti-viral antibodies. For example, almost all individuals have antibodies to measles while reovirus infections are prevalent in about half the population. [14,15] Potent anti-viral responses such as type 1 interferons (IFNs) may also inhibit viral replication within the tumour. [8] Secondly, viruses have to endure acidotic and hypoxic conditions,transverse necrotic tumour regions and areas of poor vasculature in order to survive and infect tumour cells. [1] Thereafter, the availability of cell receptors may become a limiting factor in viral entry. [8] These obstacles are expected as viruses are foreign but this does not mean they are unsuitable therapeutic agents. On the contrary, viruses have the advantage of alerting the immune system to attack their infected target(s).
Enhancing oncolytic virotherapy via protective strategies
Protective strategies are aimed at improving delivery of viruses and avoiding viral clearance. The systemic delivery of viruses can be improved by preventing uptake of viruses by liver Kupffer cells (specialised macrophage cells). In mouse studies, viral delivery can be enhanced by clodronate-containing liposomes. [1] Clodronate is a selective macrophage-depleting agent that can temporarily inhibit viral uptake by Kuppfer cells, thereby allowing more virus particles to reach the tumour site. [1] Recent interest is focused on cell-carrier based delivery of oncolytic viruses, which aims to protect viruses from systemic and intra-tumoural barriers by packaging within a cell carrier that supports viral replication and targets tumour cells, its microenvironment or the tissue/organ in which the tumour resides. [16]
Cell-carriers targeting tumour cells include tumour-infiltrating lymphocytes (TILs) and cytokine-induced killer (CIK) cells. [16] TILs are T cells which accumulate in tumours and possess T cell receptors (TCRs) that recognise tumour-associated antigens (TAAs) in the context of major histocompatibility complex (MHC). [17] Since TILs are inherently cytotoxic to T cells, using such a carrier synergistically enhances the anti-tumour effects of oncolytic viruses. Highly-specific TAAs are rare and use of less-specific TAAs may lead to non-specific targeting of normal cells. [18] Production of TILs against TAAs is also an expensive and tedious process, which argues against its widespread clinical application. [16] Conversely, although cytotoxic lymphocytes like CIKs have a lower tumour-specificity, these cells are non-MHC dependent and can proliferate ex vivo without antigen stimulation. [18] Thorne et al. injected vaccinia virus-containing CIKs into nude mice and found that the VV/CIK combination was able to accurately target tumour cells and also improved the survival rate of mice as compared to VV administration alone. [19] To improve specificity, Yoon et al. engineered Her-2/neu expressing CIKs which can target ovarian cancer cells in nude mice with high affinity. Results suggest that this approach was more effective in killing cancer cells than administering Herceptin alone. [20] Nonetheless, mechanisms underlying the tumour-specificity of CIKs remain unclear and should be studied further.
In comparison, cell carriers targeting the tumour microenvironment have well-studied. Examples include mesenchymal stem cells (MSCs) and tumour-associated macrophages (TAMs). [18] MSCs are often attracted by inflammatory chemokines expressed in the microenvironment while TAMs tend to accumulate in hypoxic areas and regions of chronic inflammation in the tumour. [16] Mader et al. reported that in mouse studies, intra-peritoneal injection of a measles virus-MSC combination can prolong the survival period of mice with ovarian cancer. [21] Similarly, a clinical study found that intravenous injection of autologous MSCs carrying the modified adenovirus-ICOVIR 5 into four children with metastatic neuroblastoma was found to induce a complete clinical response in one child who also achieved complete remission within 3 years. [22] However, as MSCs are potentially tumourigenic, there is a trade-off between exploiting its propensity for tumour accumulation and the risk of enhancing tumour growth. The main criticism against targeting the tumour microenvironment relates to the inability of these cell carriers to deliver viruses directly into tumour cells. However, modifying the microenvironment through the engineering of viruses containing genes encoding pro-apoptotic and pro-inflammatory cytokines may circumvent this limitation by disrupting tumour-promoting interactions between the microenvironment and cancer cells. [16] Furthermore, the administration of proteases such as relaxin to degrade the extracellular matrix or fusogenic membrane glycoproteins to promote cell-to-cell fusion before oncolytic therapy may facilitate intratumoural spread of viruses. [23,34]
Lastly, the targeting of tumour-associated tissues and organs is also achieved by carriers such as dendritic cells (DCs) and peripheral blood lymphocytes (PBLs). [18] These carriers are attractive because they circulate through lymphoid organs such as the lymph nodes and spleen, which are sites of micrometastases and T-cell priming. [16] DC or PBL mediated delivery of VSV and reoviruses have been shown to purge metastases in lymphoid organs. Qiao et al. found that a VSV/PBL combination partially purged B16 metastases in mice 2-3 days after administration. [25] The oncolysis of metastatic cells by VSV also primed anti-tumour T cell responses effectively and probably contributed to fast purging. [16] Targeting of tissues/organs is the least specific but this negates the requirement for highly-specific tumour markers. In addition, the circulatory paths of these cell carriers are well-characterised, allowing better prediction of their tumour trafficking patterns. [18]
The mechanisms of viral loading, amplification and transfer are equally important in enhancing cell-carrier based strategies. Willmon et al. suggested that the loading of viruses depends on the multiplicity of infection (MOI), which is the ratio of infectious agent to infection target (i.e. cell carrier). [16] In high MOI loading, a higher viral loading density may be achieved but many viral particles will be stuck to the cell’s external surface and become susceptible to neutralising antibodies. [26] Conversely, in low MOI loading, most viral particles will be internalised although the viral loading density may be lower. [26] This approach may help avoid neutralisation and is suitable for individuals who have pre-existing antibodies against the oncolytic virus (e.g. measles and reovirus).
The carrier’s ability to support viral replication determines the amount of virus delivered. As viral replication can be affected by intact IFN responses in normal cells and also requires synchronous timing with carrier bursting, tumour cells have been implicated as possible carriers. [27] A successful example has been shown in the use of VSV-infected carcinoma cells to target lung metastases in mice but safety issues concerning the tumourigenity of tumour cell-based carriers remain. [28]
The transfer of virus from cell carrier to tumour cells is crucial as exposed viral particles are susceptible to neutralisation. In some viruses such human immunodeficiency virus (HIV), viral spread is mediated by a virological synapse (a specialised form of immunological synapse) between TCRs on T cells and MHC on adjacent cells. [29] By identifying viruses which utilises a virological synapse, oncolytic viruses can transfer safely between cells.
Besides cell-carrier based strategies, immunosuppression has been considered as a means of inhibiting anti-viral immunity. In rat glioma models, cyclophosphamide and cyclosporin A (CPA) have been shown to enhance HSV-mediated oncolysis by inhibiting tumour-mediated phagocyte infiltration. [30] However, recent studies suggest that such agents can be immunostimulatory and there is increasing recognition that anti-viral immunity also contribute to effective anti-tumour responses; implying that immune mechanisms of oncolytic virotherapy may need to be examined further. [31]
Immune mechanisms of oncolytic virotherapy
The direct oncolytic effects of oncolytic virotherapy are well appreciated. Successful infection and efficient spread of oncolytic viruses determine the extent of tumour lysis; leading to emphasis on developing viruses that replicated robustly and extensively. [31] However, the lack of a straightforward dose-response relationship suggests that other oncolytic mechanisms are present. The immune system may play paradoxical roles in enhancing or impeding anti-tumour responses mediated by oncolytic viruses. [32]
Innate immune responses have been shown to inhibit viral replication in rat glioma models as indicated by rapid decrease in HSV/VV titers with concomitant increase in natural killer (NK) cell infiltration following oncolytic virotherapy. [30,33] However, viral-mediated recruitment of NK cells is advantageous as NK cells are cytotoxic and associated with tumour regression. NK cells and DCs are also involved in reciprocal interactions. [31] In vitro experiments involving Mel888 melanoma cell lines showed that reovirus-infected DCs induced IFN-β production, which in turn activated NK cells. [34] Activation of NK cells resulted in cytotoxic effects against Mel888 cells and reciprocal maturation of DCs. [34] As DCs are involved in antigen presentation to T cells, DC maturation may also promote adaptive anti-tumour responses. However, DC functions are virus-dependent as studies showed that wild-type measles and adenoviruses are inhibitory and neutral respectively. [31] It appears that the timing of viral clearance is crucial and prolonging this therapeutic window by immunosuppression may be beneficial. This is because some immunosuppressive agents may suppress anti-viral responses while stimulating anti-tumour responses. For example, similar to HSV, rat glioma studies indicate that CPA may promote VV replication while inducing a cytokine storm, which enhances activity of tumour-associated cytotoxic lymphocytes. [35]
Adaptive anti-tumour responses may be shaped by two models of immune activation: the infectious non-self (INS) and ‘danger’ models. [31] The former refers to the provision of pathogen-associated molecular patterns (PAMPs) such as viral nucleic acids to pattern-recognition receptors (e.g. toll-like receptors) on antigen-presenting cells (APCs) while the latter refers to the release of endogenous ‘danger’ signals such TAAs to APCs. [31] In the INS model, the presence of viral PAMPs induces activation and proliferation of antibodies and T cells upon antigen presentation. Infection of tumour cells is therefore not a pre-requisite for anti-tumour responses, which may instead be due to bystander effects of anti-viral responses. This was illustrated by Breitbach et al. in a murine colorectal cancer model whereby administration of HSV and VV infected only a small number of cancer cells but triggered massive destruction of non-infected cancer cells. [36] Conversely, the ‘danger’ model is more in line with oncolysis of tumour cells. Greiner et al. showed that an attenuated VV was capable of lysing human melanoma cells with subsequent development of an anti-TAA response. [37] These two models are not mutually exclusive, suggesting that the actual anti-tumour effect may be mediated by both, with their relative contributions dependent on the immunogenicity of the oncolytic virus or the tumour. [31] It is therefore apparent from an immunological perspective that effective oncolyic virotherapy may capitalise on the use of highly immunogenic viruses in a bystander effect or alternatively, promoting efficient anti-TAA responses via engineering of TAA-expressing viral vectors in poorly immunogenic viruses. [31,38]
The mechanisms involved in oncolytic virotherapy are summarised in Figure 1.
Future work
The current development of oncolytic virotherapy is based on rational designing but this approach may not always lead to the most selective and potent viruses. Buazon and Hermiston suggested that directed evolution might help researchers identify viruses with these desired characteristics. This involves growing diverse viruses in conditions that enhance diversity and passaging them through conditions mimicking the tumour microenvironment. [39] Application of directed evolution to colon cancer cell lines resulted in the adenovirus ColoAd1, which was 2-3 logs more potent than the advanced ONYX-15 and also had a therapeutic window 3-4 logs greater than the standard Ad5. [4,40] Furthermore, ColoAd1 is more sensitive to the anti-viral cidofovir (CDV) than either of its parents (Ad11p and Ad3) and this was due to directed evolution. [41] Thus, such an approach has a promising safety profile.
Integrating oncolyic virotherapy with existing treatments must be considered. Current studies have indicated promising results with radiotherapy and chemotherapy. A combination of modified HSV and radiotherapy have shown additive cell-killing effects in colorectal cancer assays and increased tumour regression in human glioma xenograft models. [42,43] It was suggested that radiotherapy could have improved viral replication and spread through irradiation-induced cellular changes. Similarly, pre-clinical studies have indicated that combination of ONXY-15 with cisplatin and 5-flurouracil in oesophageal cancers had a 39% increase in response rate as compared to chemotherapy alone (79% versus 40%). [44] Although both radiotherapy and chemotherapy are immunosuppressive to some extent, synergistic effects can be achieved by selecting the right virus and radiation/drug dosage. Combination of immunotherapy and virotherapy is at an early stage but success has been seen with VSV therapy combined with IL-2 and regulatory T cell (Treg) depletion in terms of enhanced NK cell activity and increased viral delivery. [45]
In the short term, the conflict between intra-tumoural and intravenous/intra-peritoneal administration of oncolytic viruses needs to be resolved. Mastrangelo et al showed that intra-tumoural injection of a GM-CSF-modified VV was able to induce regression in distant non-injected metastatic sites in melanoma patients but systemic effects were absent in intra-tumoural injections of ONYX-15 or reovirus. [46] Intravenous administration of the latter viruses was efficacious but resulted in thrombocytopenia and transaminitis respectively. [47] Therefore, when deciding the route of administration, a clear clinical endpoint must be established (targeting primary tumour or metastatic sites) and this will guide the type of virus used and effects (beneficial and detrimental) observed, and eventually how the patient is managed.
To conclude, oncolytic virotherapy has its antecedent in early observations and experiments detailing viral-mediated tumour regressions. Despite being neglected for decades, its resurgence reflects a current trend towards exploring new oncological treatments and a genuine hope that it can deliver better clinical outcomes. Encouraging early results and the increasing availability of solutions to its problems suggest that it is well-poised to be the avant-garde of next-generation cancer therapeutics.
Conflict of interest
None declared.
Correspondence
K Ho: koho2292@uni.sydney.edu.au
References
[1] Prestwich RJ, Errington F, Harrington KJ, Pandha HS, Selby P, Melcher A. Oncolytic Viruses: Do they have a role in anti-cancer therapy? Clin Med Oncol 2008; 2:83-96.
[2] Pelner L, Fowler GA, Nauts HC. Effects of concurrent infections and their toxins on the course of leukemia. Acta Med Scand Suppl 1958; 338: 1–47.
[3] Kelly E, Russell SJ. History of Oncolytic Viruses: Genesis to Genetic Engineering. Mol Ther 2007; 15(4):651-9.
[4] Garber K. China approves world’s first oncolyic virus therapy for cancer treatment. J Natl Cancer Inst 2006; 98:298-300.
[5] Gavhane YN, Shete AS, Bhagat AK, Shinde VR, Bhong KK, Khairnar GA, et al. Solid Tumours: Facts, Challenges and Solutions. IJPSR 2011; 2(1):1-12.
[6] McCormick F. Future prospects for oncolytic therapy. Oncogene 2005; 24:7817-9.
[7] Waldmann TA. Immunotherapy: Past, Present and Future. Nat Med 2003; 9(3):269-77.
[8] Wong HH, Lemonine NR, Wang Y. Oncolytic viruses: Overcoming the Obstacles. Viruses 2010; 2(1):78-106.
[9] Chen L, Chen D, Gong M, Na M, Li L, Wu H, et al. Concomitant use of Ad5/35 chimeric oncolytic adenovirus with TRAIL gene and taxol produces synergistic cytotoxicity in gastric cancer cells. Cancer Lett 2009; 284:141-8.
[10] Cervantes-Garcia D, Ortiz-Lopez R, Mayek-Perez N, Rojas-Martinez A. Oncolytic virotherapy. Ann Hepatol 2008; 7(1):34-45.
[11] Lu W, Zheng S, Li XF, Huang JJ, Zheng X, Li Z. Intra-tumour injection of H101, a recombinant adenovirus, in combination with chemotherapy in patients with advanced cancers: a pilot phase II clinical trial. World J Gastroenterol 2004; 10(24):3634-8.
[12] Aghi M, Martuza RL. Oncolytic viral therapies-the clinical experience. Oncogene 2005; 24:7802-16.
[13] Ganly I, Kirn D, Eckhardt G, Rodriguez GI, Soutar DS, Otto R, et al. A phase I study of Onyx-015, an E1B attenuated adenovirus, administered intratumourally to patients with recurrent head and neck cancer. Clin Cancer Res 2000; 6(3):798-806.
[14] Tyler KL. Mammalian reoviruses. In Lippencott Fields Virology, Williams and Wilkens: Philidelphia; 2001.
[15] Iankov ID, Blechacz B, Liu C, Schmeckpeper JD, Tarara JE, Federspiel MJ, et al. Infected cell carriers: a new strategy for systemic delivery of oncolytic measles in cancer virotherapy. Mol Ther 2007; 15:114-22.
[16] Wilmon C, Harrington K, Kottke T, Prestwich R, Melcher A,Vile R. Cell carriers for oncolytic viruses: Fed Ex for cancer therapy. Mol Ther 2009; 17(10):1667-76.
[17] Goff SL, Smith FO, Klapper JA, Sherry R, Wunderlich JR, Steinberg SM, et al. Tumour infiltrating lymphocyte therapy for metastatic melanoma: analysis of tumours resected for TIL. J Immunother 2010; 33(8):840-7.
[18] Su X, Zhang L. Advances in cell carriers for oncolytic viruses in cancer therapy. Tumour 2011; 31(1):85-8.
[19] Thorne SH, Negrin RS, Contag CH. Synergistic antitumour effects of immune cell-viral biotherapy. Science 2006; 331(5768):1780-84.
[20] Yoon SH, Lee JM, Woo SJ, Park MJ, Park SJ, Kim HS, et al. Transfer of Her-2/neu specificity into cytokine-induced killer (CIK) cells with RNA encoding chimeric immune receptor (CIR). J Clin Immunol 2009; 29(6):806-14.
[21] Mader EK, Maeyama Y, Lin Y, Butler GW, Russell HM, Galanis E, et al. Mesenchymal stem cell carriers protect oncolytic measles viruses from antibody neutralization in an orthotopic ovarian cancer therapy model. Clin Cancer Res 2009; 15(23):7246-55.
[22] Garcia-Castro J, Alemany R, Cascallo M, Martinez-Quintanilla J, Arriero-Mdel M, Lassaletta A, et al. Treatment of metastatic neuroblastoma with systemic oncolyic virotherapy delivered by autologous mesenchymal stem cells: an exploratory study. Cancer Gene Ther 2010; 17(7):476-83.
[23] Kim JH, Lee YS, Kim H, Huang JH, Yoon AR, Yun CO. Relaxin expression from tumour-targeting adenoviruses and its intra-tumoural spread, apoptosis induction, and efficacy. J Natl Cancer 2006; 98:1482-93.
[24] Bateman A, Bullough F, Murphy S, Emiliusen L, Lavillette D, Cosset FL, et al. Fusogenic membrane glycoproteins as a novel class of genes for the local and immune-mediated control of tumour growth. Cancer Res 2000; 60:1492-7.
[25] Qiao J, Kottke T, Willmon C, Galivo F, Wongthida P, Diaz RM, et al. Purging metastases in lymphoid organs using a combination of antigen-nonspecific adoptive T cell therapy,oncolytic virotherapy and immunotherapy. Nat Med 2008; 14(1):37-44.
[26] Kottke T, Diaz RM, Kaluza K, Pulido J, Galivo F, Wongthida P, et al. Use of biological therapy to enhance both virotherapy and adoptive T-cell therapy for cancer. Mol Ther 2008; 16:1910-8.
[27] Ottolino-Perry K, Diallo JS, Lichty BD, Bell JC, McCart JA. Intelligent design: combination therapy with oncolytic viruses. Mol Ther 2010; 18(2):251-63.
[28] Garcia-Castro J, Martinez-Palacio J, Lillo R, Garcia-Sanchez F, Alemany R, Madero L, et al. Tumour cells as cellular vehicles to deliver gene therapies to metastatic tumours. Cancer Gen Ther 2005; 12(4):341-9.
[29] Groot F, Welsch S, Sattentau QJ. Efficient HIV-1 transmission from macrophages to T cells across transient virological synapses. Blood 2008; 111:4660-3.
[30] Fulci G, Breymann L, Gianni D, Kurozomi K, Rhee SS, Yu J, et al. Cyclophosphamide enhances glioma virotherapy by inhibiting innate immune responses. Proc Natl Acad Sci 2006; 103:12873-8.
[31] Prestwich RJ, Errington F, Diaz RM, Pandha HS, Harrington KJ, Melcher AA, et al. The Case of Oncolytic Viruses Versus the Immune System: Waiting on the Judgment of Solomon. Hum Gene Ther 2009; 20(10):1119-32.
[32] Prestwich RJ, Harrington KJ, Pandha HS, Vile RG, Melcher AA, Errington F. Oncolytic viruses: a novel form of immunotherapy. Expert Rev Anticancer Ther 2008; 8(10):1581-8.
[33] Lun XQ, Jang JH, Tang N, Deng H, Head R, Bell JC, et al. Efficacy of systemically administered oncolytic vaccinia virotherapy for malignant gliomas is enhanced by combination therapy with rapamycin or cyclophosphamide. Clin Cancer Res 2009; 15:2777-88.
[34] Prestwich RJ, Errington F, Ilett EJ, Morgan RS, Scott KJ, Kottke T, et al. Tumour infection by oncolytic reovirus primes adaptive anti-tumour immunity. Clin Cancer Res 2008; 14:7358-66.
[35] Brentjens RJ, Riviere I, Hollyman D, Taylor C, Nikhamin Y, Stefanski J, et al. Unexpected Toxicity of Cyclophosphamide Followed by Adoptively Transferred CD19-Targeted T Cells in a Patient with Bulky CLL. Molecular Therapy. 2009; 17(Suppl 1):S157.
[36] Breitbach CJ, Paterson JM, Lemay CG, Falls TJ, Mcguire A, Parato KA, et al. Targeted inflammation during oncolytic virus therapy severely compromises tumour blood flow. Mol Ther 2007; 15:1686-93.
[37] Greiner S, Humrich JY, Thuman P, Sauter B, Schuler G, Jenne L. The highly attenuated vaccinia virus strain modified virus Ankara induces apoptosis in melanoma cells and allows bystander dendritic cells to generate a potent anti-tumoural immunity. Clin Exp Immunol 2006; 146:344-53.
[38] Diaz RM, Galivo F, Kottke T, Wongthida P, Qiao J, Thompson J, et al. Oncolytic immunovirotherapy for melanoma using vesicular stomatitis virus. Cancer Res 2007; 67:2840-8.
[39] Bauzon M, Hermiston TW. Oncolytic Viruses: The Power of Directed Evolution. Adv Viro 2012; doi:10.1155/2012/586389.
[40] Kuhn I, Harden P, Bauzon M, Chartier C, Nye J, Thorne S, et al. Directed evolution generates a novel oncolytic virus for the treatment of cancer treatment. PLoS ONE 2008; 3(6): e2409. doi:10.1371/journal.pone.0002409.
[41] Bauzon M, Jin F, Kretschmer P, Hermiston T. In vitro analysis of cidofovir and genetically engineered TK expression as potential approaches for the intervention of ColoAd1-based treatment of cancer. Gene Ther 2009; 16(9):1169-74.
[42] Stanziale SF, Petrowsky H, Joe JK, Roberts GD, Zager JS, Gusani NJ, et al. Ionizing radiation potentiates the antitumour efficacy of oncolytic herpes simplex virus G207 by upregulating ribonucleotide reductase. Surgery 2002; 132:353-9.
[43] Advani SJ, Sibley GS, Song PY, Hallahan DE, Kataoka Y, Roizman B. Enhancement of replication of genetically engineered herples simplex viruses by ionizing radiation: a new paradigm for destruction of therapeutically intractable tumours. Gene Ther 1998; 5:160-5.
[44] Heise C, Sampson-Johannes A, Williams A, McCormick F, Von Hoff DD, Kim DH. ONYX-15, an E1B gene-attenuated adenovirus, causes tumour-specific cytolysis and antitumoural efficacy that can be augmented by standard chemotherapeutic agents. Nat Med 1997; 3:639-45.
[45] Kottke T, Galivo F, Wongthida P, Diaz RM, Thompson J, Jevremovic D, et al. Treg depletion-enhanced IL-2 treatment facilitates therapy of established tumours using systemically delivered oncolytic virus. Mol Ther 2008; 16:1217-26.
[46] Mastrangelo MJ, Maguire HC Jr, Eisenlohr LC, Laughlin CE, Monken CE, Mccue PA, et al. Intratumoural recombinant GM-CSF-encoding virus as gene therapy in patients with cutaneous melanoma. Cancer Gene Ther 1999; 6:409-22.
[47] Liu TC, Kirn D. Systemic efficacy with oncolytic virus therapeutics: clinical proof-of-concept and future directions. Cancer Res 2007; 67(2):429-32.
 Will last year be a turning point or just another chapter in the saga of medical workforce planning in Australia? The story, so ably publicised by the high profile grassroots #interncrisis campaign, [1] AMSA and the AMA, covered the lapse of planning by jurisdictional health authorities to provide graduates from Australian medical schools with internships. [2]
Will last year be a turning point or just another chapter in the saga of medical workforce planning in Australia? The story, so ably publicised by the high profile grassroots #interncrisis campaign, [1] AMSA and the AMA, covered the lapse of planning by jurisdictional health authorities to provide graduates from Australian medical schools with internships. [2]