Background: Melioidosis is a relatively high-incidence, high-mortality tropical infectious disease caused by Burkholderia pseudomallei. To date, the few prevention and management strategies in practice have failed to reduce mortality from septic shock in patients with severe melioidosis. Up to 60.9% of patients also have pre-existing type 2 diabetes mellitus (T2DM), the most significant risk factor for melioidosis. An effective tertiary prevention strategy against melioidosis for these diabetic individuals would impact significantly on the burden of disease. Glibenclamide, a drug belonging to the sulfonylurea class and commonly used as an antidiabetic, may have the potential to be one such strategy.
Aim: To examine the underlying inflammatory cause of morbidity and mortality in melioidosis and to assess the potential for glibenclamide to ameliorate these causes.
Results: Bacteraemia with B. pseudomallei leads to widespread infection. Multi-organ damage and loss of function results from both direct bacterial damage and an excessive inflammatory response, the latter of which also causes potentially fatal septic shock in 21% of cases. Massive cellular infiltration of the lungs is particularly damaging. The immunomodulatory effects of T2DM further exacerbate the deleterious immune response into a dysregulated, hyperinflammatory state. On the other hand, the several anti-inflammatory effects of glibenclamide have been demonstrated to significantly reduce mortality from septic shock in melioidosis.
Conclusion: For diabetics living in regions where melioidosis is endemic, choosing glibenclamide over other sulfonylureas and metformin for antidiabetic treatment could be a promising tertiary prevention measure against melioidosis.
Introduction
 Melioidosis, a tropical infectious disease, is a significant cause of death and illness in northern Australia and Southeast Asia. Its non-specific prodrome and clinical presentation makes early detection difficult.[1] Yet, timely diagnosis is critical because responsiveness to treatment declines with progression of the disease over time.[2] Morbidity and mortality remains high despite aggressive antibiotic treatment. As of yet, no vaccine is available for primary prevention and novel developments such as granulocyte colony-stimulating factor (G-CSF) and corticosteroid therapy lack evidence as good measures of tertiary prevention. Considering the significant population health threat, any effective prevention strategy would be of value. This article suggests the potential use of glibenclamide, an antidiabetic sulfonylurea, for tertiary prevention of melioidosis in diabetics. Because diabetics are approximately 13 times more likely to contract melioidosis,[3,4] this strategy may have widespread application.
Melioidosis, a tropical infectious disease, is a significant cause of death and illness in northern Australia and Southeast Asia. Its non-specific prodrome and clinical presentation makes early detection difficult.[1] Yet, timely diagnosis is critical because responsiveness to treatment declines with progression of the disease over time.[2] Morbidity and mortality remains high despite aggressive antibiotic treatment. As of yet, no vaccine is available for primary prevention and novel developments such as granulocyte colony-stimulating factor (G-CSF) and corticosteroid therapy lack evidence as good measures of tertiary prevention. Considering the significant population health threat, any effective prevention strategy would be of value. This article suggests the potential use of glibenclamide, an antidiabetic sulfonylurea, for tertiary prevention of melioidosis in diabetics. Because diabetics are approximately 13 times more likely to contract melioidosis,[3,4] this strategy may have widespread application.
One of the major and dangerous end-stage complications of melioidosis is septic shock. Especially in settings such as Northeast (NE) Thailand where melioidosis is endemic but intensive care is unavailable, morbidity and mortality from septic shock are unacceptably high. Systemically-spread B. pseudomallei stimulates massive release of cytokines into the blood, this event being instrumental in the immunopathogenesis of septic systemic vasodilation, hypotension, vascular hyperpermeability, and disseminated intravascular coagulation (DIC). Furthermore, poor glycaemic control in diabetics increases the risk and severity of these events by precipitating a compensatory, dysregulated, and hyperinflammatory response to bacterial immunogenic stimuli. Demanding particular attention is the stimulated production of cytokine IL-1β because it promotes excessive neutrophilic recruitment to the lungs and bacterial persistence inside cells. Fortunately, there is strong evidence that glibenclamide acts protectively against IL-1β-mediated damage by targeting IL-1β production directly as well as multiple upstream components in the IL-1β production pathway. The result of glibenclamide use for diabetics is a significantly reduced morbidity and mortality from melioidosis septic shock compared with diabetics not taking the drug.
Epidemiology of Melioidosis
Melioidosis is endemic in Southeast Asia, northern Australia, India, Hong Kong, southern China and Taiwan.[5,6] Isolated sporadic cases have also appeared in Central America, the Caribbean, New Caledonia, Mauritius, Africa, and the Middle East.[7] Of particular concern are the hyperendemic hotspots – NE Thailand and the Top End of the Northern Territory of Australia. A 2006 NE Thailand study that gathered results from four large hospitals reported the region experienced an estimated minimum annual incidence of 21.3 cases per 100,000 people and case fatality rate of 40.5%, melioidosis locally being the third highest infectious cause of death and second most common pathogenic cause of community-acquired bacteraemia.[8,3] From 2004 to 2009, according to data collected at Royal Darwin Hospital (RDH), the annual incidence in the Top End was 21.6 per 100,000 people and average case fatality rate plateaued at 9% having decreased from 30% since 1989. The lower fatality rate in Darwin is attributed to greater access to intensive care unit (ICU) supportive care and early sepsis management that prolongs life in the event of fatal septic shock, a complication that develops in at least 21% of cases.[9]
Type 2 diabetes mellitus (T2DM) is the largest risk factor for melioidosis. 48% and 60.9% of individuals with melioidosis were confirmed to have T2DM at RDH and in NE Thailand respectively.[10,11] The 2006 Thai study reported that the relative risk (RR) of melioidosis in adult diabetics compared with non-diabetics was 12.4.[3] In the Top End region, combining diabetes with the additional risk factor of Indigenous ethnicity raised the RR from 13.1 to 20.6. Other notable risk factors associated with a significant RR are chronic lung disease (RR 4.3), age ≥ 45 years (RR 4.0), chronic renal disease (RR 3.2), Indigenous ethnicity (RR 3.0), male sex (RR 2.4) and hazardous alcohol consumption (RR 2.1).[6]
The presence of any of these risk factors in infected individuals also dramatically increases their chance of developing septic shock (RR 4.5) and death (RR 9.2), the risk factors with highest independent association with death being age ≥ 50 years (RR 2.1) and chronic lung disease (RR 1.5). Malignancy (RR 1.9) and rheumatic heart disease and/or congestive cardiac failure (RR 1.7) are statistically insignificant risk factors for death. Clinical presentations most likely to result in death are septic shock (RR 11.2) and, out of the non-septic shock cases, the presence of neurological infection foci (RR 4.7).[9] Additionally, case fatality during the peak rainfall months of December through February is 1.6 times greater than it is during other months.[9]
Immunopathogenesis and pathophysiology
Melioidosis is caused by Gram-negative bacterium B. pseudomallei. Bacteria, found in contaminated soil, rodents, food, water, and excretions, are transmitted via inhalation, ingestion, or percutaneous inoculation – usually direct contact with open skin lesions.[12,13] Post-inoculation, B. pseudomallei can invade most human cell types. Employing Type 3 Secretion System (TTSS) clusters, bacteria enter non-phagocytic cells. If bacteria are phagocytosed, TTSS enables exit from intracellular phagocytic endosomes such that degradation is evaded. Once escaped into the cytoplasm of cells both phagocytic and non-phagocytic, bacteria replicate and self-induce polarised actin filamentation that confers motility, facilitating spread to neighbouring cells by forcing host-cell membrane protrusion and fusion.[14]
B. pseudomallei possesses highly immunogenic factors that trigger a strong host immune reaction essential to the host for early bacterial containment.[15] B. pseudomallei expresses pathogen-associated molecular patterns including lipopeptides, peptidoglycan, lipopolysaccharide, flagellin, TTSS, and DNA. They are recognised by host cell toll-like receptors (TLR) and NOD-like receptors (NLR). TLRs and NLRs are expressed by immune cells both professional – macrophages and dendritic cells – and non-professional – epithelial cells, endothelial cells, and fibroblasts.[16]
Activation of NLRC4 or NLRP3 induces binding of caspase-1, Asc (apoptosis-associated speck-like protein containing CARD) and NLRC4 or NLRP3 to form an inflammasome. The NLRC4 inflammasome in infected macrophages triggers pyroptosis, serving to limit intracellular B. pseudomallei growth and proliferation, while the NLRP3 inflammasome performs proteolytic activation of pro-IL-1β and pro-IL-18 into their mature forms for secretion.[17] IL-1β recruits neutrophils to infection site(s). However, excessive recruitment is often deleterious because neutrophils, lacking NLRC4, fail to pyroptose and instead provide a favourable intracellular environment that sustains chronic bacterial persistence. In the lungs, persistence leads to damaging pulmonary abscess formation and acute respiratory distress syndrome.[17,18] In contrast, elevated IL-18 production correlates with survival and immunoprotection because IL-18 induces IFN-γ production.[17,19] IFN-γ activates macrophages, stimulating their direct antimicrobial processes – phagolysosomal fusion and toxic reactive nitrogen species synthesis that produces nitrosative stress.[20] The cytokine also facilitates macrophage antigen processing and presentation, recruits leukocytes to infection site(s), upregulates Th1 CD4+ cell population, enhances natural killer cell function, regulates B cell anti-lipopolysaccharide antibody production and isotype switching.[21]

Figure 1. NLRC4 inflammasome leads to immunoprotective effects while NLRP3 inflammasome produces both protective and deleterious responses. Glibenclamide works by inhibiting NLRP3 inflammasome formation and its deleterious effects.
TLR activation upregulates secretion of principal inflammatory mediators including type 1 interferon, chemokines, antimicrobial proteins, and pro-inflammatory cytokines.[22] Elevated expression of TLR1, TLR2, TLR3, TLR4, TLR5, TLR8, and TLR10 has been demonstrated in patients with septic melioidosis.[16] In particular, stimulation of the TLR2-mediated signalling pathway is a principal step in recognising the immune challenge of B. pseudomallei and initiating early inflammatory processes.[23] TNF-α and IL-6, along with IL-1β, increase vascular permeability, induce acute phase protein production, and recruit leukocytes to the site of infection.[24] TNF-α and IL-6 also activate the complement and coagulation cascades that are key defense mechanisms of the innate response.[25] However, excessive inflammatory cytokine production induced by widespread bacteraemia often leads to septic shock characterised by systemic vasodilatory hypotension, vascular hyperpermeability causing major cellular and fluid leakage from the intravascular to extravascular compartments, DIC, and death in the absence of immediate treatment.[26]
Through the establishment of bacteraemia, B. pseudomallei spreads from primary foci of infection to other body tissues, usually the lungs, genitourinary tract, skin, joints, bones, liver, spleen, skeletal muscles, prostate, parotid gland, and nervous system. Multi-organ spread leading to impaired organ function and failure is the main source of morbidity and mortality in melioidosis.[27] Thus, a rapid but non-deleterious inflammatory response is critical before B. pseudomallei establishes an intracellular niche that enables its persistence and protection against eradication by a subsequent immune attack. Paradoxically, subsequent immune attacks may cause further damage to the host.
Effect of type 2 diabetic state on host response
Diabetics, due to their generally immunosuppressed state, compared with non-diabetics, are more susceptible to developing sepsis from most organisms,[28] with the most common source of systemic spread being respiratory, followed by urinary and abdominal.[29] Gram-positive bacteria have become the leading cause of sepsis since the 1980s, and sepsis due to causes other than B. pseudomallei actually affects diabetics more commonly than melioidosis.[29,30] However, it is still of significance that diabetics are particularly vulnerable to pathogens such as B. pseudomallei and Mycobacterium tuberculosis because immune defence against these intracellular bacteria is highly macrophage-mediated – a function that is critically impaired in poorly-controlled T2DM.[31]
T2DM, especially if poorly controlled, causes marked immunomodulation that produces B. pseudomallei-induced immune responses that are damaging and yet insufficient to offer host protection. Morris et al. created an ex vivo whole-blood assay using human peripheral blood to compare inflammatory responses to B. pseudomallei between diabetics and non-diabetics. Immune insufficiency was worst in poorly controlled diabetics, the assay detecting: elevated serum IL-10 (an anti-inflammatory cytokine); reduced CD11b on polymorphonuclear leukocytes (PMNs) leading to decreased PMN function with reduced activation, adhesion, transmigration, and migratory capacity towards IL-8; reduced endotoxaemia-induced upregulation of ICAM-1; and defects in phagocytic detection and response to the bacteria.[32] In vivo and in vitro models using streptozotocin (STZ)-induced, leptin deficiency, leptin receptor deficiency, and diet-induced diabetic mice found similar immune impairments.[31,33-35] Transcriptional analysis of STZ-diabetic mice responses over the first 42 hours of B. pseudomallei exposure attributed delayed defence and splenic dysfunction (permitting uncontrolled bacterial replication intracellularly causing susceptibility to sepsis) to diminished TLR2 recognition of the bacterium.[34]
Incompetence of the early inflammatory response to contain an initial infection precipitates a compensatory, dysregulated, hyperinflammatory response to the spreading infection. The intensity of this ensuing reaction is exacerbated by chronic low-grade inflammation and increased oxidative stress, both characteristic of T2DM. Morris et al. found poorly controlled diabetics to have the most elevated levels of pro-inflammatory markers ESR, CRP, TNF-α, IL-1β, IL-6, IL-8, IL-12p70, MCP-1, and MPO (which indicates increased oxidative burst activity in PMNs). At focal infection sites, there was extensive infiltration with PMNs and greater risk of tissue damage, as well as generalised endothelial dysfunction and vascular inflammation.[32]
Hyperglycaemia is a major link between T2DM, immune derangement, and susceptibility to sepsis. The supra-physiological hyperosmolarity of hyperglycaemic blood directly potentiates TLR4-mediated cytokine production, as well as dampening phagocytic responses and granulocyte oxidative burst.[36] Activation of the RAGE pathway by advanced glycation end-products formed secondary to hyperglycaemia perpetuates inflammation and worsens survival in septic mice.[37] Furthermore, in the event of sepsis, poor glycaemic control allowing for periods of hyperglycaemia in both diabetics and non-diabetics correlates with longer hospital stay, greater morbidity, and possibly decreased survival.[38] In addition to immunomodulatory effects, hyperglycaemia exacerbates hypotension in septic shock by promoting glycosuric diuresis and cardiac hyperresponsiveness to cholinergic stimulation and the baroreflex.[39] Elevated risk of myocardial infarction, stroke, and venous thromboembolism is associated with the prothrombotic effect of acute hyperglycaemia that is further potentiated by hyperinsulinaemia or an inflammatory stress state.[40]
Prevention and management
No human vaccine is available.[41] CDC prevention guidelines recommend avoiding contact with soil and stagnant water in endemic regions.[42] High-risk individuals should stay indoors during heavy wind and rain in endemic regions due to possible bacterial aerosolisation that greatly facilitates transmission.[43]
Treatment involves two weeks of intravenous antibiotics – ceftazidime, meropenem, or imipenem, in combination with trimethoprim-sulfamethoxazole – followed by 3 months of oral eradication therapy to prevent recrudescence.[44] However, even with early antibiotic administration, case fatality from septicaemia remains at 37% in Thailand.[45] The development of septic shock is an indication for ICU supportive care usually involving invasive monitoring, fluid resuscitation, renal replacement therapy, and vasopressor, inotropic, and mechanical ventilatory support.[46,47]
Adjunctive use of recombinant G-CSF holds no clinical utility for improving sepsis from melioidosis and other aetiologies. Both animal and human trials – including prospective, multicentre, randomised, double-blind, and placebo-controlled studies – confirm this.[47-49] In fact, G-CSF may cause increased hepatic dysfunction and higher peak troponin I levels.[50] Other immunomodulatory adjuncts such as corticosteroids do not improve survival.[46] In light of the paucity of effective evidence-based prevention strategies and adjunct therapies for underserved populations, we turn to a novel potential for tertiary prevention.
Glibenclamide and its protective effect
Glibenclamide is a sulfonylurea used in the management of diabetes. It antagonises ATP-dependent potassium (KATP) channels in pancreatic β-cells, stimulating insulin release. The salient risk associated with glibenclamide is accidentally developing hypoglycaemia, an event of varying seriousness in patients who are not critically ill but a great predictor of mortality in acute sepsis. Furthermore, recent studies comparing glibenclamide with metformin and other sulfonylureas elucidated its significant adverse effects in addition to severe hypoglycaemia, such as increased risk of malignancy and mortality from cardiovascular disease due to interference with ischaemic preconditioning.[51,52] Despite glibenclamide still being a popular choice, a trend in medical opinion has arisen against its use in favour of alternative sulfonylureas.[53,54]
However, for T2DM individuals living in regions endemic with melioidosis, choosing glibenclamide over other antidiabetic drugs has an additional benefit that clinicians must consider. In a 5-year prospective cohort study from 2002 to 2006, Koh et al. followed 1160 adult patients with culture-confirmed melioidosis for 28 days during and after their admission to a major NE Thailand hospital. 71.3% of diabetic individuals taking glibenclamide survived from melioidosis after 28 days, while only 50.7% of diabetics not taking glibenclamide and 47.0% of non-diabetics survived (survival of patients discharged from hospital within 28 days were assumed to have survived). Using a logistics regression model, glibenclamide treatment reduced case fatality with an adjusted odds ratio (AOR) of 0.34 when compared to diabetics not taking glibenclamide and an AOR of 0.47 compared to non-diabetics. Incidences of hypotension (AOR 0.48) and respiratory failure (AOR 0.50) were also reduced in these patients.[55] Therefore, this protective effect must be factored into the drug’s risk-benefit comparison with metformin and with other sulfonylureas. If it informs clinicians’ drug choices for glycaemic control in management of T2DM, glibenclamide can contribute to tertiary prevention of melioidosis.
Although preventing hyperglycaemia in sepsis improves patient outcomes, glibenclamide does not rely on its glucose-lowering effect.[56] Using a mouse model, Koh et al. attributed the mechanism of glibenclamide’s protective effect to two main anti-inflammatory pathways. Firstly, glibenclamide reduces IL-1β secretion, attenuating IL-8 production and neutrophilic and monocytic influx into the lungs (without completely ablating the neutrophilic response).[55,57] In vitro evidence suggests that glibenclamide does this by partially blocking NLRP3 inflammasome formation and/or by directly inhibiting the secretion of mature IL-1β (Figure 1).[57-59] Glibenclamide may also attenuate transcription and translation of caspase-1, NLRP3, and IL-1β genes.[57] Secondly, by reducing systemic vasodilation and maintaining normal peripheral vascular resistance, glibenclamide restores systemic mean arterial pressure in the event of septic shock. KATP channels in vascular smooth muscle preferentially open during sepsis.[60] When they do, they hyperpolarise the cell, inhibiting Ca2+ influx (via voltage-dependent Ca2+ channels) and causing muscular relaxation. Glibenclamide opposes this effect by blocking the KATP channels. However, the only evidence for this is found in animal models.[61,62]
Conclusion
Melioidosis remains a significant public health concern due to its high incidence, mortality and case fatality rates particularly in the Top End of Northern Territory and NE Thailand. T2DM is the largest risk factor for melioidosis. The antidiabetic drug, glibenclamide, reduces morbidity and mortality from melioidosis-induced septic shock and so plays a potential role in tertiary prevention of melioidosis. In the debate over glibenclamide use, consideration of the drug’s protective effect for diabetics living in melioidosis-endemic regions, particularly those that are resource-limited, is critical.
Acknowledgements
None
Conflict of Interests
None declared
References
1. Loveleena, Chaudry R, Dhawan B. Melioidosis; the remarkable imitator: recent perspectives. J Assoc Physicians India. 2004;52:417-20.
2. Suputtamongkol Y, Hall AJ, Dance DA, Chaowagul W, Rajchanuvong A, Smith MD, et al. The epidemiology of melioidosis in Ubon Ratchatani, northeast Thailand. Int J Epidemiol. 1994;23(5):1082-90.
3. Kanoksil M, Jatapai A, Sharon PJ, Limmathurotsakul D. Epidemiology, microbiology and mortality associated with community-acquired bactaremia in Northeast Thailand: a multicenter surveillance study. PLoS One. 2013 Oct;8(1):e54714.
4. Suputtamongkol Y, Chaowagul W, Chetchotisakd P, Lertpatansuwun N, Intaranongpai S, Ruchutrakool T, et al. Risk factors for melioidosis and bacteraemic melioidosis. Clin Infect Dis. 1999;29(2):408-13.
5. Blaney DD, Gee JE, Theresa SL. Chapter 3: infectious diseases related to travel: melioidosis. Centers for Disease Control and Prevention 2011.
6. Currie BJ, Dance DA, Cheng AC. The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg. 2008;102 Suppl 1:S1-4.
7. Raja NS, Ahmed MZ, Singh NN. Melioidosis: an emerging infectious disease. J Postgrad Med. 2005;51(2):140-5.
8. Limmathurotsakul D, Wongratanacheewin S, Teerawattanasook N, Wongsuvan G, Chaisuksant S, Chetchotisakd P, et al. Increasing incidence of human melioidosis in Northeast Thailand. Am J Trop Med Hyg. 2010;82(6):1113-7.
9. Currie BJ, Ward L, Cheng AC. The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year Darwin prospective study. PLoS Negl Trop Dis. 2010;4(11):e900.
10. Parameswaran U, Baird RW, Ward LM, Currie BJ. Melioidosis at Royal Darwin Hospital in the big 2009-2010 wet season: comparison with the preceding 20 years. Med J Aust. 2012;196(5):345-8.
11. Currie BJ, Jacups SP, Cheng AC, Fisher DA, Anstey NM, Huffam SE, et al. Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop Med Int Health. 2004;9(11):1167-74.
12. Currie BJ, Jacups SP. Intensity of rainfall and severity of melioidosis, Australia. Emerg Infect Dis. 2003;9:1538-42.
13. Howe C, Sampath A, Spotnitz M. The Pseudomallei group: A review. J Infect Dis. 1971;124(6):598-606.
14. Allwood EM, Devenish RJ, Prescott M, Adler B, Boyce JD. Strategies for intracellular survival of burkholderia pseudomallei. Front Microbiol. 2011;2:170.
15. Easton A, Haque A, Chu K, Lukaszewski R, Bancroft GJ. A critical role for neutrophils in resistance to experimental infection with Burkholderia pseudomallei. J Infect Dis. 2007;195(1):99-107.
16. Wiersinga WJ, Catharina WW, Mark DC. Toll-like receptor 2 impairs host defense in Gram-Negative sepsis caused by Burkholderia pseudomallei (melioidosis). PLoS Med. 2007;4(7):e248.
17. Ceballos-Olvera I, Sahoo M, Miller MA, Del Barrio L, Re F. Inflammasome-dependent pyroptosis and IL-18 protect against Burkholderia pseudomallei lung infection while IL-1β is deleterious. PLoS Pathog. 2011;7(12):e1002452.
18. Koh GC, Schreiber MF, Bautista R, Maude RR, Dunachie S, Limmathurotsakul D, et al. Host responses to melioidosis and tuberculosis are both dominated by interferon-mediated signaling. PLoS ONE. 2013;8(1):e54961. doi:10.1371/journal.pone.0054961.
19. Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1334-49.
20. Flynn JL, Chan J. Immune evasion by Mycobacterium tuberculosis: living with the enemy. Curr Opin Immunol. 2003;15(4):450-5.
21. Boehm U, Klamp T, Groot M, Howard JC. Cellular responses to interferon-gamma. Annu Rev Immunol. 1997;15:749-95.
22. Wiersinga WJ, van der Poll T, White NJ, Day NP, Peacock SJ. Melioidosis: insights into the pathogenicity of Burkholderia pseudomallei. Nat Rev Microbiol. 2006;4(4):272-82.
23. Chin CY, Monach DM, Nathan S. Genome wide transcriptome profiling of a murine acute melioidosis model reveals new insights into how Burkholderia pseudomallei overcomes host innate immunity. BMC Genomics. 2011;11:672.
24. Takeuchi O, Akira S. Pattern recognition receptors and inflammation. Cell. 2010;149(6):805-20.
25. Wiersinga WJ, Currie BJ, Peacock SJ. Melioidosis. N Engl J Med. 2012;367(11):1035-44.
26. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions of sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644-55.
27. Meumann EM, Cheng AC, Ward L, Currie BJ. Clinical features and epidemiology of melioidosis pneumonia: results from a 21-year study and review of the literature. Clin Infect Dis. 2012;54:362-9.
28. Muller LMAJ, Gorter KJ, Hak E, Goudzwaard WL, Schellevis FG, Hoepelman AIM, et al. Increased risk of common infections in patients with type 1 and type 2 diabetes mellitus. Clin Infect Dis. 2005;41:281-8.
29. Martin GS. Sepsis, severe sepsis and septic shock: changes in incidence, pathogens and outcomes. Expert Rev Anti Infect Ther. 2012;10(8):701-6.
30. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546-54.
31. Hodgson KA, Morris JL, Feterl ML, Govan BL, Ketheesan N. Altered macrophage function is associated with severe Burkholderia pseudomallei infection in a murine model of type 2 diabetes. Microbes Infect. 2011;13(14-15):1177-84.
32. Morris J, Williams N, Rush C, Govan B, Sangla K, Norton R, et al. Burkholderia pseudomallei triggers altered inflammatory profiles in a whole-blood model of type 2 diabetes-melioidosis comorbidity. Infect Immun. 2012;80(6):2089-99.
33. Williams NL, Morris JL, Rush C, Govan BL, Ketheesan N. Impact of streptozotocin-induced diabetes on functional responses of dendritic cells and macrophages towards Burkholderia pseudomallei. FEMS Immunol Med Microbiol. 2011 Mar;61(2):218-27.
34. Chin CY, Monack DM, Nathan S. Delayed activation of host innate immune pathways in streptozotocin-induced diabetic hosts leads to more severe disease during infection with Burkholderia pseudomallei. Immunology. 2012;135(4):312-32.
35. Hodgson KA, Govan BL, Walduck AK, Ketheesan N, Morris JL. Impaired early cytokine responses at the site of infection in a murine model of type 2 diabetes and melioidosis comorbidity. Infect Immun. 2013;81(2):470-7.
36. Wade CE. Hyperglycemia may alter cytokine production and phagocytosis by means other than hyperosmotic stress. Crit Care. 2008;12(5):182.
37. Bopp C, Bierhaus A, Hofer S, Bouchon A, Nawroth PP, Martin E, et al. Bench-to-bedside review: The inflammation-perpetuating pattern-recognition receptor RAGE as a therapeutic target in sepsis. Crit Care. 2008;12(1):201.
38. Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449-61.
39. Liu IM, Chang CK, Juang SW, Kou DH, Tong YC, Cheng KC, et al. Role of hyperglycaemia in the pathogenesis of hypotension observed in type-1 diabetic rats. Int J Exp Pathol. 2008;89(4):292-300.
40. Lemkes BA, Hermanides J, Devries JH, Holleman F, Meijers JC, Hoekstra JB. Hyperglycemia: a prothrombotic factor? J Thromb Haemost. 2010;8(8):1663-9.
41. Patel N, Conejero L, De Reynal M, Easton A, Bancroft GJ, Titball RW. Development of vaccines against Burkholderia pseudomallei. Front Microbiol. 2011;2:198.
42. Centers for Disease Control and Prevention (CDC). Melioidosis: prevention. Atlanta: CDC; 2012.
43. Australian Centre for Disease Control. Melioidosis. Darwin: ACDC; 2012.
44. Currie B, Anstey N. Treatment and prognosis of melioidosis. UpToDate; 2012.
45. White NJ, Dance DA, Chaowagul W, Wattanagoon Y, Wuthiekanun V, Pitakwatchara N. Halving of mortality of severe melioidosis by ceftazidime. Lancet. 1989;2(8665):697-701.
46. Panomket P, Chetchotisakd P, Sermswan RW, Pannengpetch P, Wongratanacheewin S. Use of a low-dose steroid as an adjunct in the treatment, in mice, of severe sepsis caused by Burkholderia pseudomallei. Ann Trop Med Parasitol. 2009;103(7):635-46.
47. Mohammad RA. Use of granulocute colony-stimulating factor in patients with severe sepsis or septic shock. Am J Health Syst Pharm. 2010;67(15):1238-1245.
48. Cheng AC, Stephens DP, Anstey NM, Currie BJ. Adjunctive granulocyte colony-stimulating factor for treatment of septic shock due to melioidosis. Clin Infect Dis. 2004;38(1):32-7.
49. Cheng AC, Limmathurotsakui D, Chierakul W, Getchalarat N, Wuthiekanun V, Stephens DP, et al. A randomized controlled trial of granulocyte colony-stimulating factor for the treatment of severe sepsis due to melioidosis in Thailand. Clin Infect Dis. 2007;45(3):308-14.
50. Stephens DP, Thomas JH, Higgins A, Bailey M, Anstey NM, Currie BJ, et al. Randomized, double-blind, placebo-controlled trial of granulocyte colony-stimulating factor in patients with septic shock. Crit Care Med. 2008;36(2):448-54.
51. Monami M, Balzi D, Lamanna C, Barchielli A, Masotti G, Buiatti E, et al. Are sulphonylureas all the same? A cohort study on cardiovascular and cancer-related mortality. Diabetes Metab Res Rev. 2007;23(6):479-84.
52. Schramm TK, Gislason GH, Vaag A, Rasmussen JN, Folke F, Hansen ML, et al. Mortality and cardiovascular risk associated with different insulin secretagogues compared with metformin in type 2 diabetes, with or without a previous myocardial infarction: a nationwide study. Eur Heart J. 2011;32(5):1900-8.
53. WHO Expert Committee. The selection and use of essential medicines. World Health Organ Tech Rep Ser. 2008;(950):backcover, vii-174.
54. Riddle MC. Editorial: sulfonylureas differ in effects on ischaemic preconditioning – is it time to retire glyburide? J Clin Endocrinol Metab. 2003;88(2):528-30.
55. Koh GC, Maude RR, Schreiber MF, Limmathurotsakul D, Wiersinga WJ, Lee SJ, et al. Glyburide is anti-inflammatory and associated with reduced mortality in melioidosis. Clin Infect Dis. 2011;52(6):717-25.
56. Koh GC, Weehuizen TA, Breitbach K, Krause K, de Jonh HK, Kager LM, et al. Glyburide reduces bacterial dissemination in a mouse model of melioidosis. PLoS Negl Trop Dis. 2013;7(10):e2500.
57. Kewcharoenwong C, Rinchai D, Utispan K, Suwannasaen D, Bancroft GJ, Ato M, et al. Glibenclamide reduces pro-inflammatory cytokine production by neutrophils of diabetes patients in response to bacterial infection.
58. Lamkanfi M, Mueller JL, Vitari AC, Misaphi S, Fedorova A, Deshayes K, et al. Glyburide inhibits the Cryopyrin/Nalp3 inflammasome. J Cell Biol. 2009;187(1):61-70.
59. Hamon Y, Luciani MF, Becq F, Verrier B, Rubartelli A, Chimini G. Interleukin-1beta secretion is impaired by inhibitors of the Atp binding cassette transporter, ABC1. Blood. 1997;90(8):2911-5.
60. Sorrentino R, d’Emmanuele di Villa Bianca R, Lippolis L, Sorrentino L, Autore G, Pinto A. Involvement of ATP-sensitive potassium channels in a model of a delayed vascular hyporeactivity induced by liposaccharide in rats. Br J Pharmacol. 1999;127(6):1447-53.
61. Vanelli G, Hussain SN, Aguggini G. Glibenclamide, a blocker of ATP-sensitive potassium channels, reverses endotoxin-induced hypotension in pig. Exp Physiol. 1985;80(1):167-70.
62. Landry DW, Oliver JA. The ATP-sensitive K+ channel mediates hypotension in endotoxaemia and hypoxic lactic acidosis in dog. J Clin Invest. 1992;89(6):2071-4.


 As a university academic whose professional interests include the chemistry of serious reactor accidents I disagree with many of
As a university academic whose professional interests include the chemistry of serious reactor accidents I disagree with many of




 Psychotic disorders are characterised by the presence of symptoms that reflect an excess or distortion of normal functions. For example, hallucinations, delusions, thought disorder and disorganised behaviour are symptoms characteristic of psychosis. Patients diagnosed with schizophrenia must demonstrate positive symptoms or severe negative symptoms (e.g. flattened affect, social withdrawal) in addition to deterioration in their social and vocational functioning. [1] Hence, the diagnosis is typically made after the onset of significant symptomology.
Psychotic disorders are characterised by the presence of symptoms that reflect an excess or distortion of normal functions. For example, hallucinations, delusions, thought disorder and disorganised behaviour are symptoms characteristic of psychosis. Patients diagnosed with schizophrenia must demonstrate positive symptoms or severe negative symptoms (e.g. flattened affect, social withdrawal) in addition to deterioration in their social and vocational functioning. [1] Hence, the diagnosis is typically made after the onset of significant symptomology.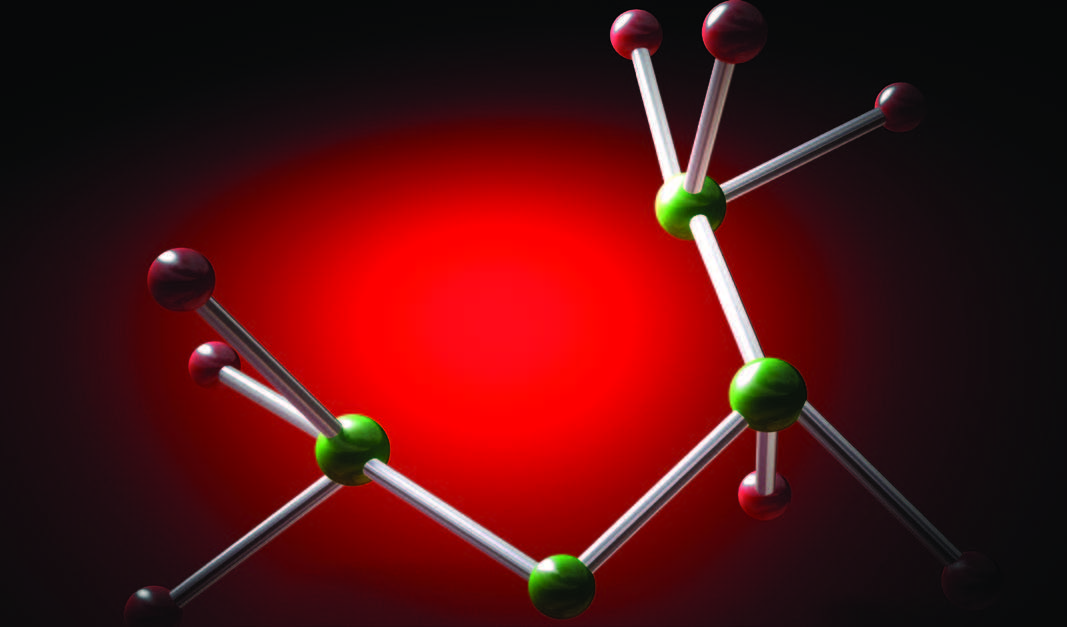
 γ-aminobutyric acid (GABA) is the major inhibitory neurotransmitter in the brain and is responsible for regulating neuronal excitability. There are at least three different receptors that it targets — GABAA, GABAB and GABAC. [1] The GABAA receptor is the main target for the popular class of drugs, the benzodiazepines. This receptor is an ionotropic membrane receptor, which facilitates the movement of chloride into cells. In neurons, this increases the threshold needed to excite them.[2] Benzodiazepines are positive modulators at this receptor and exert their effects by binding to the interface between the γ2 and α subunits on the GABAA receptor. [3] Since they are modulators and not agonists, they do not work in the absence of GABA. [4] They only bind to the receptors containing the α5, α3, α2, and α1 subunits. [5] Each of these subunits mediates different effects. In knockout mice, the α1 subunit has shown hypnotic/sedative effects, whilst the α3, α2 and α5 subunits have anti-anxiolytic effects and these have been exploited for therapeutic use.[6]
γ-aminobutyric acid (GABA) is the major inhibitory neurotransmitter in the brain and is responsible for regulating neuronal excitability. There are at least three different receptors that it targets — GABAA, GABAB and GABAC. [1] The GABAA receptor is the main target for the popular class of drugs, the benzodiazepines. This receptor is an ionotropic membrane receptor, which facilitates the movement of chloride into cells. In neurons, this increases the threshold needed to excite them.[2] Benzodiazepines are positive modulators at this receptor and exert their effects by binding to the interface between the γ2 and α subunits on the GABAA receptor. [3] Since they are modulators and not agonists, they do not work in the absence of GABA. [4] They only bind to the receptors containing the α5, α3, α2, and α1 subunits. [5] Each of these subunits mediates different effects. In knockout mice, the α1 subunit has shown hypnotic/sedative effects, whilst the α3, α2 and α5 subunits have anti-anxiolytic effects and these have been exploited for therapeutic use.[6]
 I am writing to discuss an interesting construct in psychiatry often referred to as ‘psychopathy’. In psychiatry there is often
I am writing to discuss an interesting construct in psychiatry often referred to as ‘psychopathy’. In psychiatry there is often
 John was wheeled into hospital on a Friday of a long weekend. He was elderly and frail, with severe Parkinson’s disease. Many
John was wheeled into hospital on a Friday of a long weekend. He was elderly and frail, with severe Parkinson’s disease. Many


