Background: Australia has the highest incidence of skin cancer in the world. Despite decades of public health campaigns, these figures are rising, particularly within the male population.
Aim: This study aimed to establish whether a gender divide exists in relation to skin cancer awareness, prevention and early detection in a rural area of Australia where skin cancer rates are high.
Methods: Participants were recruited from two medical practices in the Northern Rivers region. Skin cancer awareness, knowledge and prevention were assessed through a qualitative questionnaire, with some questions having responses that used a modified Likert scale. Participant responses were scored for correctness and unpaired t-tests were used to compare scores between the genders.
Results: Females scored higher than males in all three domains assessed, including awareness, knowledge and prevention. Knowledge surrounding skin cancer awareness was significantly higher (p=0.03) in females compared to males. Similarly, the frequency at which females performed skin self-examinations was significantly higher (p= 0.04) than their male counterparts. Males were less likely than females to participate in a range of sun-protective behaviours, however, similar rates of sunscreen use were observed in both genders.
Conclusions: Overall, our study demonstrated that females from the Northern Rivers, NSW were more knowledgeable about skin cancer than their male counterparts and are more likely to participate in sun protective behaviours and secondary prevention strategies, including skin self-examinations and clinical skin examinations by a medical practitioner. These findings of a gender divide are supported by several international studies and can perhaps provide an explanation as to why a discrepancy exists between Australian males and females with regard to the increased incidence of skin cancer.
Introduction
 Australia has the highest incidence of skin cancer in the world, with two out of three Australians being diagnosed before the age of 70. [1] There are three types of skin cancer related to sun exposure: malignant melanoma (MM), basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Malignant melanoma is the least common but the most serious, accounting for 75% of skin cancer related deaths. [2] Early melanomas are usually highly visible and previous studies have shown that early detection of thin lesions is associated with a high five-year survival rate. [3, 4] BCC is the most common skin cancer in Australia, followed by SCC. [5] Although the non-melanoma skin cancers rarely result in mortality, they are very common and have the potential to recur, disfigure and metastasise if not identified and treated in a timely manner. [6, 7]
Australia has the highest incidence of skin cancer in the world, with two out of three Australians being diagnosed before the age of 70. [1] There are three types of skin cancer related to sun exposure: malignant melanoma (MM), basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Malignant melanoma is the least common but the most serious, accounting for 75% of skin cancer related deaths. [2] Early melanomas are usually highly visible and previous studies have shown that early detection of thin lesions is associated with a high five-year survival rate. [3, 4] BCC is the most common skin cancer in Australia, followed by SCC. [5] Although the non-melanoma skin cancers rarely result in mortality, they are very common and have the potential to recur, disfigure and metastasise if not identified and treated in a timely manner. [6, 7]
The epidemiological literature concerned with predisposing factors for skin cancer emphasises the considerable influence of ultraviolet (UV) radiation on the incidence of skin cancer. [8, 9] Primary prevention efforts are aimed at reducing the risk factors for skin cancer, most notably sun exposure and sunburn, through environmental changes, social changes and behavioural modification. [5] This includes diverse activities to minimise exposure to the sun, such as adopting sun protection strategies such as using sunscreen, wearing protective clothing and avoiding midday sun. [10 11]
Secondary prevention efforts to reduce skin cancer, including the early detection through systematic skin cancer screening and excision of early precancerous or cancerous lesions, have an important impact on the morbidity and mortality associated with skin cancer. [12] The 2003 SCREEN project (Skin Cancer Research to Provide Evidence for the Effectiveness of Screening) in Northern Germany demonstrates the feasibility and effectiveness of systematic skin cancer screening. Over a twelve-month period, physicians carried out 360,288 skin checks and consequently identified 3103 melanomas resulting in a 34% increase in melanoma incidence for the year of the study. Five years after SCREEN, melanoma mortality was reduced by over 50%. [13] Northern Germany has a low skin cancer prevalence compared to Australia, thus the anticipated benefits of systematic skin cancer screening are likely to be even greater in Australia.
Current Australian clinical guidelines do not recommend systematic skin cancer screening, however, the Australasian College of Dermatologists recommends annual skin checks by a physician in individuals who are at an increased risk of developing skin cancer. [14] Risk factors for skin cancer include host factors such as Fitzpatrick skin types I and II, multiple melanocytic naevi or dysplastic naevi and melanoma in a first degree relative. [15] Environmental risk factors include excessive UV exposure and frequent sunburns, particularly from a young age. In addition to annual screening of high-risk groups, it is recommended that the general population perform whole body skin self-examinations (SSE) at least four times a year. [14] Previous surveys on the practice of SSE in Australia have indicated varying results, ranging from 6-60% of the population practising some kind of SSE depending on the population studied. [16] A survey of Queensland residents found that the rates of SSE were higher among females compared to males and there was an increased likelihood of SSE in individuals with a higher level of education. [17]
It has long been known that UV radiation is a significant factor in the development of skin cancer. As a result of this well documented link, the Australian government has launched numerous public health campaigns since the 1980’s. [18] These sun safe media campaigns, including the well-known ‘slip, slop, slap’ campaign, aimed to increase community awareness. Despite these campaigns, the incidence of skin cancer in Australia has risen steadily over the past two decades. This rise can be partly explained by the increased diagnosis of small SCC’s and BCC’s that have previously remained untreated, however, it cannot solely be responsible for the increase in incidence.
A study by Staples et al (2006), found that rates of BCC and SCC increased from 1985 to 2006, with 70% of men and 58% of women aged over 70 years having at least one skin cancer at the later time point. [19] Further, research into the cause of this increase identified that the rates of skin cancer in males may be the primary contributor to the rise. [19, 20] Skin Cancer Australia found that the incidence of melanoma in males has risen by 100% over the last 20 years. [20] The exact cause of this increase in Australia is unclear.
It has traditionally been assumed that men have higher rates of skin cancer primarily because they are more likely than women to have outdoor jobs, which involve extensive sun exposure. This may be only one of the factors contributing to their higher risk. A recent American skin cancer foundation survey revealed that men are less likely than women to make an effort to protect themselves from the sun and are less knowledgeable when it comes to skin cancer prevention, awareness and early detection. [20] Furthermore, a qualitative study, which assessed skin cancer awareness, attitudes and sun protection behaviour among medical students at the University of Miami, Florida, found significant gender differences in sun protection and skin cancer knowledge. More women than men valued the importance of sun protection and acknowledged that sun exposure is the most important risk factor for skin cancer. [21]
A gap exists in the literature as to whether a similar gender divide is present in Australia, which could possibly explain the increased rates of skin cancers seen in the male population. Through the use of a qualitative questionnaire, this study aimed to:
- Establish whether a gender divide in relation to skin cancer knowledge and prevention exists in the Northern Rivers region of NSW, an area close to the Queensland border, where the highest rates of skin cancer in Australia have been reported. [22]
- Use these results as the basis for further studies that can better inform medical practice in relation to skin cancer awareness and prevention.
Methods
Participants and Study Design:
Participants were recruited through information posters placed in the waiting rooms of two medical practices in the Northern Rivers region: the Goonellebah Medical Centre and the Lennox Head Medical Practice. Participation in the project was voluntary and anonymous, with participants returning the completed questionnaires to a secured box placed in the waiting room. There were no exclusion criteria other than participants needing to be aged 18 years or over. The study ran between December 2012 and February 2013 inclusive.
All participants completed the qualitative questionnaire, which was largely adapted from the Department of Health and Aging – Evaluation of National Skin Cancer Awareness Campaign [23] and previous UOW research. [24] Questions were constructed in such a way as to assess knowledge and attitudes towards skin cancer awareness, prevention and early detection. The questionnaire included questions on a modified Likert scale which were adapted from a previous study. [24] Demographic information including gender, age and level of education was also collected.
Ethics:
This study received approval by the Human Research Ethics Committee (HREC) of the University of Wollongong, Australia (Ethics number: GSM12/055).
Statistical analysis:
Descriptive statistical analyses were performed to establish the distribution of participants’ characteristics. Responses either used a modified Likert scale or were scored for correctness (Appendix 1). Analyses of patients’ sun protection practices, skin cancer awareness, skin cancer knowledge, frequency of skin self-examination and skin examination with a medical practitioner were completed using EXCEL, Microsoft (Redmond, Washington, U.S) software for Windows. Recorded information was then further analysed to establish whether responses varied between genders. Sample sizes for each analysis varied slightly due to incomplete questionnaires. Analysis was performed using unpaired t-tests, with the level of significance set at p=0.05.
Results
Demographics:
In total, 91 patients from the two medical practices completed the questionnaire. There was an approximate 1.3:1 female to male ratio with a high representation of the older 55+ years age group. The age distributions of participants are shown in table 1. There is a sizeable difference in age distribution between males and females. This is largely due to the patient population seen at both medical practices. Level of education was relatively evenly distributed with 61% of females having tertiary education and 39% having secondary education compared to 58% and 42% respectively, for males.



Skin cancer knowledge:
Skin cancer knowledge was assessed through three primary domains; awareness of prevalence of skin cancer within Australia (Figure 1), knowledge surrounding types of skin cancers (Figure 2) and awareness of sunburn as a primary contributory factor for the development of skin cancer (Figure 3). Females scored significantly higher in relation to prevalence of skin cancer, and sunburn risk compared with males (Table 2). The percentage of females who correctly identified key elements in the three domains was higher than males for skin cancer prevalence (71% females; 51% males), awareness of skin cancer types – SCC (71% females; 50% males) and melanoma (77% females; 52% males), as well as sunburn as a primary contributing factor (92% females; 76% males). The percentage of males and females who correctly identified BCC as a type of skin cancer was similar (88% females; 90% males).

Reported sun protective behaviours are shown in Figure 4. The most sizeable gender differences were that more females reported using wide brimmed hats, actively seeking shade and using sunglasses. Overall, only a small percentage of participants reported not engaging in any form of sun protective behaviour (males 3%, females 2%).
Skin cancer early detection:
The frequencies of skin self-examinations are shown in Figure 5. Overall, the frequency at which females perform SSE was significantly higher than their male counterparts (p=0.04) when the response options were converted to a modified Likert scale of 0 – 3. Among females, 42% reported performing SSE frequently compared with 30% of males. The percentage of males who never (13%) or rarely (26%) performed a SSE was higher than females (8% and 6%, respectively).
The frequencies of skin examinations performed by a medical practitioner are shown in Figure 6. A substantial proportion of the male cohort (28%) reported to having never had their skin examined by a medical practitioner. This is higher than the corresponding female group (8%). Rates of reported examinations on a 6-12 month basis were much higher among the female population (38%) compared to the male population (18%). When these response options of frequency were converted to a modified Likert scale of 0-4, and compared using unpaired t-tests, there was no significant difference between males and females (p = 0.111).
Discussion
This population-based survey documents skin cancer knowledge, prevention and early detection in a Northern Rivers population (Northern NSW, Australia), an area close to the Queensland border, where skin cancer rates are high and rising rapidly particularly among the male population. The response rate obtained (n=91) was a satisfactory representation of gender (57% female, 43% male), but slightly weighted towards older age groups (>55 years). The predominantly elderly patient population seen at the two medical practices can explain this higher proportion of elderly participants.
In this population, females were significantly more knowledgeable than males in the identification of skin cancer prevalence (p=0.03) and were more likely to identify types of skin cancers, however, this difference was not significant (p=0.21). Despite Australia being a world leader in skin cancer incidence, only half (51%) of the male cohort compared to 71% of females correctly identified skin cancer incidence as being very common, occurring in 2 in 3 Australians. Given the higher prevalence of all skin cancer types within the male population , [20] this is an important finding as it suggests that perhaps skin cancer campaigns are not having as great of an impact on the male population in terms of education, and need to be more targeted in their approach.
[caption id="attachment_3960" align="aligncenter" width="300"] Figure 3. Awareness of sunburn as a key risk factor in the development of skin cancer.
Figure 3. Awareness of sunburn as a key risk factor in the development of skin cancer.



A more perturbing finding was that males scored lower than females in relation to knowledge of the types of skin cancers that exist. Only half of the male cohort correctly identified melanoma (52%) and SCC (50%) as skin cancers, compared to 77% and 71% respectively of the female cohort. These results are alarming given that melanoma is the fourth most common cancer in Australia and its incidence in the male population is 2-fold higher than that observed in females. [22] Surprisingly, and contrary to the former findings, 90% of male participants correctly identified BCC as a type of skin cancer, similar to females (88%). The exact cause of the higher identification of BCC as a skin cancer is unknown, but may be attributed to the fact that BCC is the most common and prevalent skin cancer in Australia, and thus the male population may be more familiar with its presentation. [5] Interestingly, moles (37%), age spots (18%), freckles (13%) and acne (2%) were identified by a portion of the male population as types of skin cancers.
Despite demonstrating limited knowledge in terms of skin cancer incidence and types of skin cancers, the majority of the male cohort (76%) correctly identified excessive UV exposure and in particular recurrent sunburn as a key causative factor of skin cancer. This high response rate may be a reflection of the decades of public health campaigns the Australian public have been exposed to, which highlight the well-known link between sun exposure and skin cancer. Although the male score in this area was higher than that seen in the other two domains, it was still significantly lower (p=0.033) than that of the female cohort and once again demonstrated a gender divide concerning skin cancer knowledge.
Sunscreen was the most commonly used measure of sun protection by males with 57% of the male cohort reporting the use of SPF >30 sunscreen on a regular basis. This trend is in keeping with current literature, which reports that sunscreen is the most commonly used measure of sun protection in adults. [25] Stanton et al. report that females have a greater desire for a tan and have an increased perception that a tan is healthy and this translates into them using sunscreen at lower rates then the male population. [26] Our results demonstrate no such gender difference regarding this behaviour, and in fact our study demonstrates that females are more likely than males to participate in other sun protective behaviours such as wearing a wide brimmed hat, long sleeved shirt, actively seeking shade and wearing sunglasses. Overall, females were found to be more proactive when it comes to protecting themselves from the sun, however, on a whole, the level of sun protective behaviours in both cohorts were relatively low with just over half of the female population participating in some kind of sun protective behavior on a regular basis with lower rates seen in the male population. This finding is particularly relevant, as even though the majority of these participants were in their mid to late teens when the well known ‘slip, slop, slap’ campaign was launched, a large proportion of them are not necessarily adopting sun protective behaviours.
Secondary prevention strategies include clinical systematic skin examinations by a doctor and skin self-examinations. The current Australian clinical guidelines do not recommend clinical systematic skin examinations, however, due to the high incidence of skin cancer seen in Australia, the Australasian College of Dermatologists recommends annual skin checks by a physician in individuals who are at increased risk of skin cancer. [14] The College also recommended that all individuals perform SSE at least four times a year. Overall, females were more likely than their male counterparts to have their skin examined by a physician on an annual basis, however this difference was statistically insignificant (p=0.11). In addition, 28% of males reported to never having had their skin checked by a physician compared to only 8% of females. A similar trend was observed in the frequency of SSE. The reported frequency of SSE was significantly higher in females than males (p=0.040). Furthermore, the percentage of the male cohort that never (13%) or rarely (26%) performed SSE was much higher then the female cohort. The reasons behind this difference are not fully understood and are thought to be multifactorial, with some studies suggesting that men are less likely to get their skin examined by a doctor as they are less likely to identify themselves as at risk of skin cancer and are less likely to recognise suspicious lesions which require further investigation. [27] As nearly one third of men had never had their skin examined by a doctor or rarely perform SSE, they are at increased risk of premalignant or malignant lesions going unnoticed and progressing to aggressive cancer. It is therefore important that treating physicians recognise that males are less likely to get routine skin checks and that they need to be opportunistic during a consultation and educate the patient regarding skin cancer awareness and prevention.
Strengths and Limitations
A key strength of this qualitative study is that it addresses an important clinical area where the evidence base is weak. Although the study included 91 participants, we acknowledge the limitation of recruiting from only two medical practices in the Northern Rivers region. Furthermore, the difference in the age distribution between males and females may have influenced results. There is a high representation of the 55+ age group and males in the 18-20 ‘risk taking’ age group. This is representative of the patient population seen at the two practices but may not necessarily be a true representation of the patient population of the Northern Rivers Region. Future studies with a multivariate design to extract cofounding factors of sun protective behavior and interactions between attitudes and knowledge should extend these findings to larger, more diverse samples.
Clinical implications
This study has implications for both primary care physicians and public health campaigns such as the National Skin Cancer Awareness Campaign. Many of the male participants were unaware or had limited knowledge around types of skin cancers, adopting sun protective behaviours and secondary prevention strategies. Our data suggests several key areas of skin cancer awareness that can be targeted in future research and health promotion on both a local and national level.
Conclusion
Overall, our study demonstrates that females from the Northern Rivers, NSW are more knowledgeable about skin cancer than their male counterparts and are more likely to participate in sun protective behaviours and secondary prevention strategies, including skin self-examinations and clinical skin examinations by a medical practitioner. These findings of a gender divide are supported by several other international studies and can perhaps provide an explanation as to why a discrepancy exists in Australia with regard to the increased incidence of skin cancer observed within the male population. Increasing awareness of skin cancer within the male population, encouraging them to readily adopt sun protective behaviors and encouraging them to take notice of any changing or newly appearing skin lesions with regular review and follow up by a physician, has the potential to reduce skin cancer morbidity and mortality in Australia.
Acknowledgements
The author would like to thank Dr Naomi Piyaratna for her contribution to survey development and data collection and Dr Theresa Larkin from the Graduate School of Medicine, Wollongong University for her expertise and assistance in producing this research article.
Conflict of interest
The authors declare no conflicts of interest.
References
[1] Australian Institute of Health and Welfare 2008, Cancer in Australia an overview [Internet] 2008 [cited 2012 Aug 10]. Available from: http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=6442454588
[2] Bastuji-Garin S, Diepgan T. Cutaneous malignant melanoma, sun exposure, and sunscreen use: epidemiological evidence. British Journal of Dermatology. 2002; 146 (61):24-30.
[3] Wingo P, Ries L, Rosenberg H, Miller D, Edwards C. Cancer incidence and mortality, 1973-1995: a report card for the U.S. Cancer. 1998; 82:1197-1207.
[4] Chang A, Karnell L, Menck H. The National Cancer Data Base report on cutaneous and non-cutaneous melanoma: a summary of 84836 cases from the last decade. Cancer. 1988; 83:1664-1678.
[5] National Health and Medical Research Council (NHMRC). Primary prevention of skin cancer in Australia [Internet]. 1996 [cited 2012 Oct 09]. Avaliable from: http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/hp8.pdf
[6] Randle H. Basal cell carcinoma. Identification and treatment of the high risk patient. Dermatol Surg. 1996; 22:255-261.
[7] Demetrius R, Randle H. High risk nonmelanoma skin cancers. Dermatol Surg. 1998;24:1272-1292.
[8] Turner M. Sun safety: avoiding noonday sun, wearing protective clothing and the use of sunscreen. Journal of the National Cancer Institute. 1998;90: 1854–1855.
[9] Skin Cancer Foundation. New survey reveals gender divide surrounding skin cancer awareness and prevention. [Internet]. 2012 [cited 2012 September 09]. Avaliable from: http://www.skincancer.org/media-and-press/press-release-2012/survey
[10] Dummer R, Maier T. UV protection and skin cancer. Recent results cancer res. 2002;160:7-12.
[11] Naylor M, Farmer K. The case for sunscreens: A review of their use in preventing actinic damage and neoplasia. Arch Dematol. 1997;133:1146-1154.
[12] Oliveria S, Christos P, Marghoob A, Helpern A. Skin cancer screening and prevention in the primary care setting. 2001;16:297-301.
[13] Breitbart E, Waldman A, Nolte S. Systematic skin cancer screening in Northern Germany. J Am Acad Dermatol. 2012; 66:201-211.
[14] Australasian College of Dermatologists. How to check your skin moles. [Internet]. 2004 [cited 2012 Nov 23]. Avaliable from: http://www.dermcoll.asn.au/public/a-z_of_skin-how_to_check_your_skin_moles.asp
[15] Berwick M, Eredi F, Hay J. Melanoma epidemiology and public health. Dermatol Clin. 1999;27:205-214.
[16] Aitken J, Janda M, Lowe J, Elwood M, Ring I. Prevelence of whole-body skin self-examination in a population at high risk of skin cancer (Australia). Cancer causes and control. 2004;15:453-463.
[17] Balanda P, Lowe J, Stanton R, Gillepsie M. Enhancing the early detection of melanoma within current guidelines. Aust. J. Public Health. 1994;18:420-423.
[18] Sinclair C, Foley P. Skin cancer prevention in Australia. British Journal of Dermatology. 2009;109(3):116-123.
[19] Staples M, Elwood M, Burton R, Williams J. Non-melanoma skin cancer in Australia: the 2002 national survey and trends since 1985. Medical Journal Australia. 2006;184:6–10.
[20] Cancer Australia. Skin Cancer. [Internet]. 2010 [cited 2012 Oct 09]. Avaliable from: http://www.canceraustralia.gov.au/sites/default/files/images/Factsheets/Skin_Cancer_Factsheet.pdf
[21] Patel S, Nijhawan R, Stechschulte S, Parmet J. Skin cancer awareness, attitude, and sun protection behavior among medical students at the University of Miami Miller School of Medicine. Arch Dematol. 2010;146:797-800.
[22] Queensland Cancer Registry and Queensland Cancer Fund. Cancer in Queensland. Incidence and Mortality; 2005
[23] Department of Health and aging. Evaluation of the National skin cancer awareness campaign – Third phase (2009-2010). [Internet]. 2010 [cited 2012 Aug 10]. Avaliable from: http://www.skincancer.gov.au/internet/skincancer/publishing.nsf/Content/B31B922E2431D53FCA25782A00175847/$File/eval10.pdf
[24] Khan I. Evaluating public awareness about skin cancer [Internet]. 2010 [cited 2012 Oct 09]. Avaliable from:. https://vista.uow.edu.au/webct/urw/tp0.lc20663/cobaltMainFrame.dowebct
[25] Weinstock M, Rossi J, Redding C, Maddock J. Sun protection behaviors and stages of change for the primary prevention of skin cancer among beachgoers in southeastern New England. Annals of Behavioural Medicine. 2000;22:286-293.
[26] Stanton W, Janda M, Baade P, Anderson P. Primary prevention of skin cancer: a review of sun protection in Australia and internationally. Health Promot Int. 2004;19:369-378.
[27] Janda M, Baade P, Youl P, Aitken J, Whiteman K. The skin awareness study: Promoting thorough skin self-examination for skin cancer among men 50 years or older. Contemporay Clinical Trials. 2010;21:119-130.
Appendix



 Functional specialisation of human cerebral cortex has been demonstrated in vivo using positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) [e.g. 1]. Current research is aimed at precise anatomical localisation of functionally defined areas. However, accurate localisation of active regions is an ongoing challenge given the poor spatial resolution of functional imaging and inter-individual variability in the complex morphological structure of cerebral cortex [2,3]. Consequently, location of cortical areas must be examined within an individual to obtain precise structure-function information.
Functional specialisation of human cerebral cortex has been demonstrated in vivo using positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) [e.g. 1]. Current research is aimed at precise anatomical localisation of functionally defined areas. However, accurate localisation of active regions is an ongoing challenge given the poor spatial resolution of functional imaging and inter-individual variability in the complex morphological structure of cerebral cortex [2,3]. Consequently, location of cortical areas must be examined within an individual to obtain precise structure-function information. 




 Adequate hip muscle strength is required to control the alignment of the lower limb and therefore limit exposure of distal structures to potentially damaging forces. [1] Deficits in hip muscle strength have demonstrated an association with pain and (re)injury in the hip, [2,3] knee, [4,5] and ankle. [6] Consistent with these observations, strengthening of hip muscles through exercise interventions has been shown to reduce lower limb pain and injury, [7,8] improve lower limb landing alignment, and minimise potentially injurious positions. [9] Given this well established link between hip muscle strength impairment, pain, and (re)injury; a reliable, clinically applicable means of measuring hip muscle function is necessary to assist clinicians in the development and monitoring of interventions aimed at minimising pain and (re)injury, and improving patient function.
Adequate hip muscle strength is required to control the alignment of the lower limb and therefore limit exposure of distal structures to potentially damaging forces. [1] Deficits in hip muscle strength have demonstrated an association with pain and (re)injury in the hip, [2,3] knee, [4,5] and ankle. [6] Consistent with these observations, strengthening of hip muscles through exercise interventions has been shown to reduce lower limb pain and injury, [7,8] improve lower limb landing alignment, and minimise potentially injurious positions. [9] Given this well established link between hip muscle strength impairment, pain, and (re)injury; a reliable, clinically applicable means of measuring hip muscle function is necessary to assist clinicians in the development and monitoring of interventions aimed at minimising pain and (re)injury, and improving patient function.


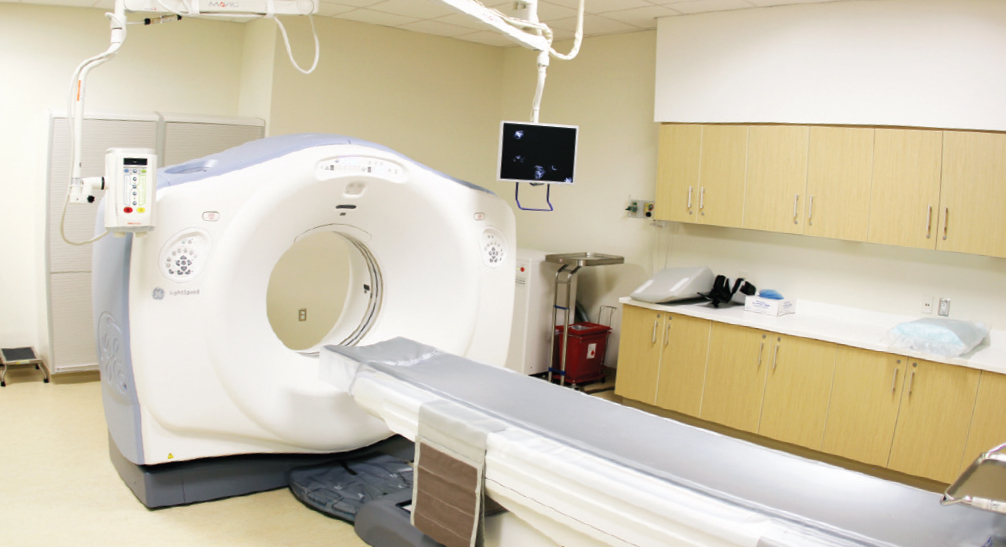
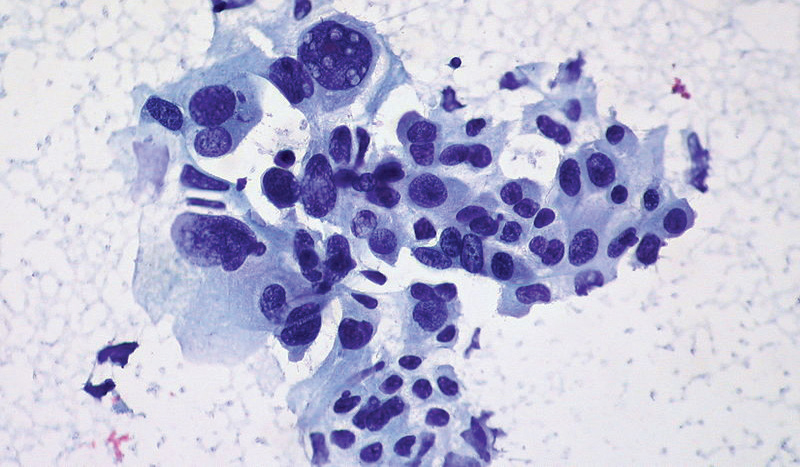
 The adrenal glands (AG), locoregional lymph nodes, and the liver are common sites of metastases in cancer patients, with more than half of adult malignancies from renal cell carcinomas affecting the AG. [1-3] The majority of AG metastases are identified on computed tomography (CT) imaging. [1,4-8] Occasionally, one may encounter primary adrenal tumours such as adrenal adenomas and rarely, adrenal carcinomas. [3,6] It is important for clinicians to be able to accurately identify the AG in cancer patients to allow early identification and subsequent management of metastases. [9-12] As there are often delays in the time for CT scans to be assessed by a radiologist, early diagnosis of adrenal metastases by physicians may be of benefit in terms of earlier treatment and cost savings. [4,13] Furthermore, physicians who are able to quickly identify adrenal lesions on CT and provide detailed information to their patients in clinic may aid their patients in the understanding of their illness. This may potentially improve treatment outcomes, especially for patients with metastatic cancer. [13-16]
The adrenal glands (AG), locoregional lymph nodes, and the liver are common sites of metastases in cancer patients, with more than half of adult malignancies from renal cell carcinomas affecting the AG. [1-3] The majority of AG metastases are identified on computed tomography (CT) imaging. [1,4-8] Occasionally, one may encounter primary adrenal tumours such as adrenal adenomas and rarely, adrenal carcinomas. [3,6] It is important for clinicians to be able to accurately identify the AG in cancer patients to allow early identification and subsequent management of metastases. [9-12] As there are often delays in the time for CT scans to be assessed by a radiologist, early diagnosis of adrenal metastases by physicians may be of benefit in terms of earlier treatment and cost savings. [4,13] Furthermore, physicians who are able to quickly identify adrenal lesions on CT and provide detailed information to their patients in clinic may aid their patients in the understanding of their illness. This may potentially improve treatment outcomes, especially for patients with metastatic cancer. [13-16]













 BB is a 73-year-old Caucasian male who presented to the Mental Health Unit (MHU) following a request and recommendation (under the Queensland Mental Health Act 2000) in response to concerns from family and friends. BB presented from a nursing home with paranoid delusions that incorporated persecutory themes with thoughts that the nursing staff were poisoning his food in order to kill him. He also presented with auditory hallucinations complaining of hearing people through a speaker telling him they were going to cut off his toes and genitals. BB expressed suicidal ideation to escape, however, no previous attempts at suicide or self-harm had been made. When BB was further questioned about a suicidal plan he stated that he would like to do it cleanly with towels around him so there was no mess but no instrument or method was established. There was no history of substance abuse.
BB is a 73-year-old Caucasian male who presented to the Mental Health Unit (MHU) following a request and recommendation (under the Queensland Mental Health Act 2000) in response to concerns from family and friends. BB presented from a nursing home with paranoid delusions that incorporated persecutory themes with thoughts that the nursing staff were poisoning his food in order to kill him. He also presented with auditory hallucinations complaining of hearing people through a speaker telling him they were going to cut off his toes and genitals. BB expressed suicidal ideation to escape, however, no previous attempts at suicide or self-harm had been made. When BB was further questioned about a suicidal plan he stated that he would like to do it cleanly with towels around him so there was no mess but no instrument or method was established. There was no history of substance abuse.
 One famous discovery of a targeted drug treatment is imatinib, a tyrosine kinase inhibitor (TKI) used to treat a subset of chronic myelogenous leukaemia expressing the Philadelphia chromosome. This discovery has triggered a series of research efforts, shedding light on topics such as tumourigenesis and cell signaling pathways, leading to the development of many new drugs which target these specific mechanisms. However, it has been documented that resistance to these drugs can develop, therefore reducing their treatment potential [1,2] This is also true for a similar group of TKIs known as epidermal growth factor receptor (EGFR) inhibitors, which have been used as part of the treatment regime for a subgroup of lung cancer patients with non-small cell lung carcinoma. This article will review the mechanisms of intrinsic and acquired resistance to EGFR inhibitors and strategies to overcome them.
One famous discovery of a targeted drug treatment is imatinib, a tyrosine kinase inhibitor (TKI) used to treat a subset of chronic myelogenous leukaemia expressing the Philadelphia chromosome. This discovery has triggered a series of research efforts, shedding light on topics such as tumourigenesis and cell signaling pathways, leading to the development of many new drugs which target these specific mechanisms. However, it has been documented that resistance to these drugs can develop, therefore reducing their treatment potential [1,2] This is also true for a similar group of TKIs known as epidermal growth factor receptor (EGFR) inhibitors, which have been used as part of the treatment regime for a subgroup of lung cancer patients with non-small cell lung carcinoma. This article will review the mechanisms of intrinsic and acquired resistance to EGFR inhibitors and strategies to overcome them. 

