The prescription of opioids is increasing worldwide, including in Australia. Consequently, opioid dependence – one of several harms associated with chronic opioid therapy – is now a growing concern. However, the risk factors for iatrogenic opioid dependence are not well understood in an Australian context. The available Australian evidence for these risks are reviewed and supplemented with data from the United States. Substance use disorder, mental disorder, pain severity and several demographic factors are associated with increased risk of opioid dependence. Factors originating within the health system, such as prescribed dose, chronicity, monitoring systems and physician attitudes may also contribute to patients developing dependence. Australian data represents a significant gap in the knowledge, and there is a need for good quality studies examining Australian populations.
The rate of opioid prescribing both in Australia and worldwide has increased dramatically. [1-3] Opioid-like analgesic dispensing in Australia increased 53% between 2002 and 2009, with tramadol and oxycodone showing the largest increases. [1] This prescribing pattern is of concern since chronic opioid therapy is associated with multiple harms, including dependence and accidental overdose. [4,5] In the USA, prescription opioid-related deaths increased 68% between 1999 and 2003, [6] with the highest risk of death in patients who were prescribed high dose opioid therapy. [7] This trend has been mirrored to a lesser extent in Australia, with an increase in oxycodone-related deaths but not morphine-related deaths. [2] There is evidence that harms related to opioid therapy are increasing as a result of increased prescriptions. [2,8]
Iatrogenic dependence can be described as physician initiated inadvertent dependence. [9] The risk of iatrogenic opioid dependence is unknown and estimates differ greatly between acute and chronic settings. [4,10,11] In addition, opioid therapy trials tend to focus on efficacy and exclude individuals at high risk of dependence. [12] Despite these limitations, studies of patients taking chronic opioid therapy found a 35% lifetime prevalence of dependence. [4,13] As a consequence, iatrogenic opioid dependence is of concern for health professionals and balancing benefits with risk of dependence is a key clinical issue. [8,14,15]
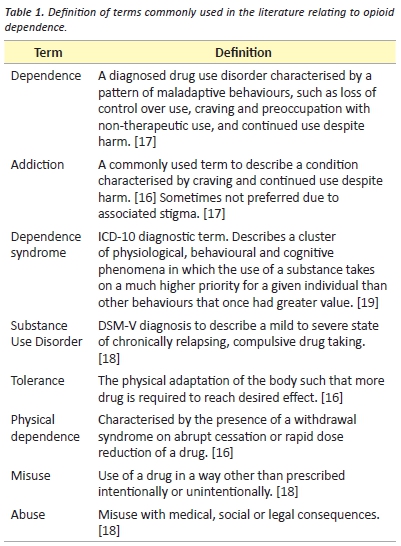
The terminology used to define and describe the use of opioids is controversial. [16,17] There are two main diagnostic systems for the diagnosis of drug use disorders internationally. The DSM-V describes “substance use disorder” as a mild to severe state of chronically relapsing, compulsive drug taking. [18] The International Classification of Diseases (ICD-10) defines a “dependence syndrome” as a cluster of physiological, behavioural and cognitive phenomena in which the use of a substance takes on a much higher priority for a given individual than other behaviours that once had greater value. [19] Addiction is a term widely used by the general public, health professionals and in the literature. [17] It is described as a chronic condition characterised by behaviours such as compulsive use, continued use despite harm and craving. [16] It has been argued that the term “addiction” represents a variety of social and cultural constructs and is often value-laden. [17] For this reason, the term “dependence” is often preferred. [17] In this article, dependence will be used to describe a diagnosed drug use disorder. Readers should view dependence as distinct from physical dependence, tolerance, abuse and misuse, which are clarified in Table 1.
Guidelines for the prescription of opioids are conflicting, with confusion around safety and efficacy. [20,21] The United States has the highest rates of opioid use in the world and multiple reviews have examined the potential risk factors for addiction. [22,23] However, differences in prescribing, demographics and health system characteristics indicate that a review in an Australian context is of value. [1] This article summarises the available Australian evidence on the risk of iatrogenic opioid dependence, supplemented with studies from the US. Four major groups of patient risk factors are described: substance abuse disorder, mental disorder, pain severity and demographic factors. The role of dependence risk screening tools is briefly assessed.Finally, the contribution of specific health system and prescribing factors is discussed.
Methods
A literature search of publications relating to risk factors for prescription opioid dependence was undertaken. The databases PubMed, CINAHL and Ovid were searched for publications published between 2004 and 2014. The search terms “Opioid OR Opiate” and “Dependence OR Addiction” and “Prescription” and “Risk” were used. This search yielded 205 publications. Additional articles were obtained from bibliographic searching. 39 relevant articles were included. 166 articles were excluded as they studied heroin use or focused on harms other than dependence, such as abuse or misuse.
Patient factors that increase risk
Substance use disorder
Despite substance abuse being a strong predictor for opioid dependence, Australian data on the relationship is lacking. Cross- sectional studies from the United States demonstrate a strong correlation between substance abuse disorder and chronic opioid use. [24,25] In addition, evidence suggests that opioid dependence is more likely in those with a past or current substance abuse disorder. [4,8,26,27] This is consistent with a longitudinal study in which a diagnosis of non-opioid substance abuse was the strongest predictor of opioid dependence in those commencing opioid therapy. [15] Recent studies also demonstrate an association between smoking and opioid dependence, with one citing smoking as the most frequently reported risk factor in their cohort. [28,29] No Australian studies were found that examined this relationship. However, the Australian National Drug Strategy Household Survey reported that 36% of recent users of opioids for non-medical reasons also used cannabis and 25% had used alcohol. [30] This data should be interpreted cautiously, as it does not reveal if the use was chronic or acute, or the reasons for use. At best it shows a tendency for opioids to be used with other psychoactive substances.
Mental disorders
Mental disorders increase the risk of iatrogenic opioid dependence. This is demonstrated by the fact that prescription opioid use is greater for patients with depression and anxiety. [25] Furthermore, these patients were prescribed opioids in higher doses and for longer durations than patients without a mental disorder. [24] Patients with mental disorders also have a higher incidence of chronic non-cancer pain. [24] Whether chronic pain is the cause or result of mental disorders is unknown; some evidence suggests the relationship is bidirectional. [24] Whether more opioids are prescribed to these patients on the basis of their higher reported pain remains to be established.
The outcomes of opioid treatment for patients with mental disorders are not well characterised as these patients are usually excluded from clinical trials. [31] However, several studies show that mental disorders are significantly associated with opioid dependence. [4,8,15,26,27,29,32] Furthermore, having two comorbid mental disorders increases the risk of addiction compared to a single mental disorder. [8] One study found a correlation between PTSD severity and opioid use, suggesting that severity of symptoms may also be implicated. [33]
Despite the increased risk of opioid dependence with mental disorders, one longitudinal study of fifteen thousand veterans with chronic prescription opioid use in the United States showed that only 3% of pain patients with comorbid mental disorders progressed to opioid abuse or dependence. [15] This highlights that the presence of a mental disorder alone cannot predict a patient’s risk of developing dependence to a prescribed opioid. There is a lack of Australian data establishing a link between mental disorders and opioid dependence.
Patient demographics
There are a number of demographic factors that may increase the risk of a patient developing opioid dependence. Studies conducted in the US have identified younger age as a strong predictor of opioid dependence, with individuals under 65 showing increased risk. [4,8,15] In Australia, the National Drug Strategy Household Survey (NDSHS) found that use of opioids for non-medical purposes was highest in persons ages 20-29. [30] As in other substance use disorders, men are more likely to develop opioid abuse or dependence than women. [8,15,26] This is consistent with NDSHS, which found that men were more likely to use pharmaceuticals for non-medical purposes in their lifetime. [30] Several other factors such as living rurally and early age of exposure to nicotine, alcohol and other drugs are significantly associated with opioid dependence. [27] In addition, a family history of substance use disorder and time spent in jail may increase the risk. [26] Being divorced, single or separated and childhood emotional trauma are also associated with opioid dependence. [4,15] It is possible that these factors interrelate and are thus more likely to occur together, compounding the risk.
A recent Australian study analysed data from the Bettering the Evaluation and Care of Health (BEACH) program, which collects data on interactions patient consultations in general practice. It found that Commonwealth Concession Card holders had a significantly higher rate of opioid prescribing compared to other patients. [34] This data poses an interesting question as to why opioid prescribing in this population is higher. Possibilities include increased willingness of doctors to prescribe and lack of access to alternative treatments such as physiotherapy.
Pain severity
The severity of a patient’s pain may contribute to opioid addiction. [35] Persistent use of opioids for chronic pain is associated with severe or very severe reported pain. [36] In addition, opioid-dependent individuals show a greater degree of pain-related limitation and greater pain severity. [4,26] This may be because addiction lowers the pain tolerance, or that a lower pain threshold confers an increased risk of addiction. [26,37] Alternatively, people experiencing greater pain severity may simply be prescribed higher doses of opioids. This could also be due to opioid-induced hyperalgesia, a state of nociceptive sensitization caused by exposure to opioids. [38] This can be mistaken for tolerance, which may result in a higher dose of opioids prescribed and thus an increased risk of addiction. No Australian studies were found examining the relationship between pain severity and increased risk of addiction.
Screening for risk
Ultimately, established risk factors should be used to create reliable screening strategies. While that is considered good practice, there is no one screening procedure that can identify chronic pain patients at risk of opioid dependence. [21,22] A common issue is the overlap of behaviours also seen in patients with undertreated pain, such as demand for higher dose medications, and taking medication in a way other than prescribed (defined as misuse). [22] This is further complicated by the fact that established risk factors have been found to be poorly associated with aberrant drug behaviours. [29]
The Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R, https://www.painedu.org/soapp.asp) tool is a self- administered 24-item tool assessing common risk factors for opioid misuse, abuse and dependence. [39] The items assess mood, attitudes towards treatment, personality traits and substance use disorder. [39] A recent study found the SOAPP score to be the strongest predictor of dependence in a cohort of patients using over the counter and prescription painkillers. [40] In addition, Butler et.al found the SOAPP-R to be reliable and valid across two different chronic pain patient populations. [39,41] However, the usefulness of SOAPP-R in a primary health care setting remains to be determined. [39]
The American Society of Interventional Pain Physicians does not recommend the use of formal dependence risk screening tools. [21] In their recent guidelines for responsible opioid prescribing, they suggest that risk stratification can be achieved through a comprehensive physician’s assessment. [21] This should include psychosocial history, functional status, psychological evaluation, substance abuse history and physical exam. [21]
Health system factors contribute to risk
In addition to patient factors, there are multiple health system factors that contribute to prescription opioid dependence. These are prescribing dose, duration of therapy, monitoring systems and physician attitudes.
Few studies have examined the relationship between dose and duration of therapy and risk of dependence. However, in a large cross-section study of individuals with a new episode of chronic non-cancer pain, those prescribed high morphine equivalent dose (120 mg), chronic (>90 days) opioid therapy were 50 times more likely to develop dependence than those on low dose acute therapy. [8] This is consistent with a recent study, which found the odds ratio for developing dependence with high dose, chronic opioid use was 122.45. [11] While the rate of high dose chronic opioid prescription in this sample was relatively low (0.1% of chronic pain patients), it represents a number needed to harm of 16.7. [8] Given the significant negative consequences of opioid dependence this number needed to harm may be unacceptable. Multiple studies found that duration of opioid therapy was more important than daily dose in determining risk of dependence. [8,11,42] Indeed, data suggests that other risk factors such as younger age and comorbid mental disorders contributed less to the risk than dose and chronicity alone. [8] This is supported by another study which found that greater than 211 days of prescribed opioids was more predictive of dependence than 90-211 days. [15] Importantly, this also suggests that the association between risk and chronicity is a linear relationship. In Australia stronger formulations account for the minority of opioids prescribed. [2] However, more research into the relationship between opioid dose, chronicity and dependence is required.
One of the goals of responsible opioid prescribing is adequate monitoring, due to the consequences of duration mentioned above. [5,21] Existing monitoring systems in Australia cannot track opioid prescriptions and supply down to the individual patient level. [5] The Pharmaceutical Benefit Schedule (PBS) data set generates a Medicare file, which can potentially identify patients misusing opioids. [5]
However, no information is included in the PBS record if a patient pays the entire cost of the medication. [5] Lack of access to comprehensive information can contribute to inappropriate prescribing. [43] Thus, a real-time prescription coordination program making use of technology would be greatly beneficial. [43]
Physician attitudes towards opioid analgesics may also profoundly impact on treatment. [14] In a mailed survey to General Practitioners in Ontario, GPs who did not believe many patients became addicted to opioids also prescribed more opioids. [14] Furthermore, over 10% of GP’s were not confident in their skills prescribing opioids. [14]. Surveys of Australian physicians studying attitudes to the use of opioids are required. Regardless of the attitude of physicians towards opioid prescription, there remains a responsibility to manage patients’ pain effectively. It is well recognised that this poses an ethical dilemma to the treating physician and involves a careful balance of risk and benefit. [9, 44] Several guidelines are available to clinicians to increase their confidence in prescribing opiate analgesics, including the RACP [45] and Hunter New England guidelines. [46]
Conclusion
It is apparent that individuals with highest risk of iatrogenic dependence will possess a constellation of risk factors. A combination of young age, depression, psychotropic medications and pain impairment combined with substance use history predicted greatest increased risk for opioid dependence. [4] However, methods for screening risk remain unreliable, compounded by a lack of universal guidelines to guide practice. In addition, high dose, chronicity, monitoring systems and physician attitudes may also increase the risk of dependence in the population. Thus far, Australian studies into opioid use have described trends in prescribing practices. Studies examining risk factors for iatrogenic opioid dependence represent a significant gap in the knowledge. Further research is likely to help guide clinicians to make better-informed decisions around opioid prescribing.
Acknowledgements
None.
Conflict of interest
None declared.
Correspondence
H Hartman: hannah.hartman@my.jcu.edu.au
References
[1] Hollingworth SA, Symons M, Khatun M, Loveday B, Ballantyne S, Hall WD, et al. Prescribing databases can be used to monitor trends in opioid analgesic prescribing in Australia. Aust N Z J Public Health. 2013;37(2):132-8.
[2] Roxburgh A, Bruno R, Larance B, Burns L. Prescription of opioid analgesics and related harms in Australia. Med J Aust. 2011;195(5):280.
[3] Olsen Y, Daumit GL, Ford DE. Opioid prescriptions by US primary care physicians from 1992 to 2001. J Pain. 2006;7(4):225-35.
[4] Boscarino JA, Rukstalis M, Hoffman SN, Han JJ, Erlich PM, Gerhard GS, et al. Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction. 2010;105(10):1776-82.
[5] The Royal Australasian College of Physicians. Prescription Opioid Policy: Improving management of chronic non-malignancy pain and prevention of problems associated with prescription opioid use. 2009. From https://www.racp.edu.au/page/policy-and-advocacy/ public-health-and-social-policy.
[6] Paulozzi LJ, Ryan GW. Opioid analgesics and rates of fatal drug poisoning in the United States. Am J Prev Med. 2006;31(6):506-11.
[7] Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85-92.
[8] Edlund MJ, Martin BC, Russo JE, Devries A, Braden JB, Sullivan MD. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic non- cancer pain: the role of opioid prescription. Clin J Pain. 2014 Jul;30(7):557-64.
[9] McLellan AT, Turner B. Prescription opioids, overdose deaths, and physician responsibility. JAMA. 2008;300(22):2672-3.
[10] Wasan A, Correll D, Kissin I, O’Shea S, Jamison R. Iatrogenic addiction in patients treated for acute or subacute pain: a systematic review. J Opioid Manag. 2005;2(1):16-22.
[11] Edlund MJ, Martin BC, Russo JE, DeVries A, Braden JB, Sullivan MD. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: the role of opioid prescription. Clin J Pain. 2014;30(7):557-64.
[12] Juurlink DN, Dhalla IA. Dependence and addiction during chronic opioid therapy. J Med Toxicol. 2012;8(4):393-9.
[13] Boscarino JA, Rukstalis MR, Hoffman SN, Han JJ, Erlich PM, Ross S, et al. Prevalence of prescription opioid-use disorder among chronic pain patients: comparison of the DSM-5 vs. DSM-4 diagnostic criteria. J Addict Dis. 2011;30(3):185-94.
[14] Wenghofer EF, Wilson L, Kahan M, Sheehan C, Srivastava A, Rubin A, et al. Survey of Ontario primary care physicians’ experiences with opioid prescribing. Can Fam Physician. 2011;57(3):324-32.
[15] Edlund MJ, Steffick D, Hudson T, Harris KM, Sullivan M. Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non- cancer pain. Pain. 2007;129(3):355-62.
[16] Savage SR, Joranson DE, Covington EC, Schnoll SH, Heit HA, Gilson AM. Definitions related to the medical use of opioids: evolution towards universal agreement. J Pain Symptom Manage. 2003;26(1):655-67.
[17] Larance B, Degenhardt L, Lintzeris N, Winstock A, Mattick R. Definitions related to the use of pharmaceutical opioids: Extramedical use, diversion, non-adherence and aberrant medication-related behaviours. Drug Alcohol Rev. 2011;30(3):236-45.
[18] American Psychiatric Association. Desk Reference to the Diagnostic Criteria from DSM-5. Washington, DC: American Psychiatric Publishing 2013.
[19] World Health Organisation. International Classification of Disease 2010 [29/04/2014]. Available from: http://apps.who.int/classifications/icd10/browse/2010/en.
[20] Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113-30. e22.
[21] Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2–guidance. Pain Physician. 2012;15(3 Suppl):S67-116.
[22] Sehgal N, Manchikanti L, Smith HS. Prescription opioid abuse in chronic pain: a review of opioid abuse predictors and strategies to curb opioid abuse. Pain Physician. 2012;15(3):ES67-ES92.
[23] Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part I–evidence assessment. Pain Physician. 2012;15(3 Suppl):S1-65.
[24] Edlund MJ, Martin BC, Devries A, Fan M-Y, Braden JB, Sullivan MD. Trends in use of opioids for chronic non-cancer pain among individuals with mental health and substance use disorders: the TROUP study. Clin J Pain. 2010;26(1):1-8.
[25] Sullivan MD, Edlund MJ, Zhang L, Unützer J, Wells KB. Association between mental health disorders, problem drug use, and regular prescription opioid use. Arch Intern Med. 2006;166(19):2087-93.
[26] Liebschutz JM, Saitz R, Weiss RD, Averbuch T, Schwartz S, Meltzer EC, et al. Clinical factors associated with prescription drug use disorder in urban primary care patients with chronic pain. J Pain. 2010;11(11):1047-55.
[27] Cicero TJ, Lynskey M, Todorov A, Inciardi JA, Surratt HL. Co-morbid pain and psychopathology in males and females admitted to treatment for opioid analgesic abuse. Pain. 2008;139(1):127-35.
[28] Zale EL, Dorfman ML, Hooten WM, Warner DO, Zvolensky MJ, Ditre JW. Tobacco smoking, nicotine dependence, and patterns of prescription opioid misuse: results from a nationally representative sample. Nicotine Tob Res. 2014 Oct 25.
[29] Layton D, Osborne V, Al-Shukri M, Shakir SAW. Indicators of drug-seeking aberrant behaviours: the feasibility of use in observational post-marketing cohort studies for risk management. Drug Safety. 2014;37(8):639-50.
[30] Australian Institute of Health and Welfare. 2007 National Drug Strategy Household Survery: detailed findings Canberra AIHW, 2008.
[31] Kalso E, Allan L, Dellemijn PL, Faura CC, Ilias WK, Jensen TS, et al. Recommendations for using opioids in chronic non-cancer pain. Eur J Pain. 2003;7(5):381-6.
[32] Mackesy-Amiti ME, Donenberg GR, Ouellet LJ. Prescription opioid misuse and mental health among young injection drug users. Am J Drug Alcohol Abuse. 2015;41(1):100-6.
[33] Meier A, Lambert-Harris C, McGovern MP, Xie H, An M, McLeman B. Co-occurring prescription opioid use problems and posttraumatic stress disorder symptom severity. Am J Drug Alcohol Abuse. 2014;40(4):304-11.
[34] Harrison CM, Charles J, Henderson J, Britt H. Opioid prescribing in Australian general practice. Med J Aust. 2012;196(6):380-1.
[35] Chang Y-P, Compton P. Management of chronic pain with chronic opioid therapy in
patients with substance use disorders. Addict Sci Clin Pract. 2013;8(1):21.
[36] Fredheim OMS, Mahic M, Skurtveit S, Dale O, Romundstad P, Borchgrevink PC. Chronic pain and use of opioids: A population-based pharmacoepidemiological study from the Norwegian Prescription Database and the Nord-Trøndelag Health Study. PAIN®. 2014;155(7):1213-21.
[37] Compton P, Charuvastra VC, Kintaudi K, Ling W. Pain responses in methadone- maintained opioid abusers. J Pain Symptom Manage. 2000;20(4):237-45.
[38] Raffa RB, Pergolizzi JV. Opioid-induced hyperalgesia: is it clinically relevant for the treatment of pain patients? Pain Manag Nurs. 2013;14(3):e67-e83.
[39] Butler SF, Fernandez K, Benoit C, Budman SH, Jamison RN. Validation of the revised screener and opioid assessment for patients with pain (SOAPP-R). J Pain. 2008;9(4):360-72.
[40] Elander JP, Duarte JM, Maratos FAP, Gilbert PF. Predictors of painkiller dependence among people with pain in the general population. Pain Med. 2014;15(4):613-24.
[41] Butler SF, Budman SH, Fernandez KC, Fanciullo GJ, Jamison RN. Cross-validation of a screener to predict opioid misuse in chronic pain patients (SOAPP-R). J Addict Med. 2009;3(2):66-73.
[42] Edlund MJMDP, Martin BCP, Russo JEP, DeVries AP, Braden JBP, Sullivan MDMD. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: the role of opioid prescription. Clin J Pain. 2014;30(7):557-64.
[43] Nicholas R, Roche A, Dobbin M, Lee N. Beyond the paper trail: using technology to reduce escalating harms from opioid prescribing in Australia. Aust N Z J Public Health. 2013;37(2):139-47.
[44] Coffin P, Banta-Green C. The dueling obligations of opioid stewardship. Ann Intern Med. 2014;160(3):207-8.
[45] The Royal Australasian College of Physicians. Prescription opioid policy. 2009. Available from: www.racp.edu.au/docs/default-source/advocacy-library/prescription-opioid-policy.pdf
[46] Hunter New England Local Health District. Pain practice guidelines. Available from: www.hnehealth.nsw.gov.au/pain/health_professionals/medical_practice_guidelines