The medical student’s first lanyard represents much more than a device which holds clinical identification cards – it symbolises their very identity, first as medical students and eventually as medical practitioners. The lanyard allows access to hospitals and a ready way to discern who’s who in a fast paced environment. It is the magic ticket that allows us to wander hospital corridors (often aimlessly) without being questioned.
Despite this, the utility of the lanyard as a symbol of “an insider” is being questioned, with mounting evidence showing it to be a harbour for the indirect transmission of bacteria from health care staff to patients. It may be time for the lanyard, like the white coat before it, to be retired as a symbolic but potentially harmful relic of the past. This essay investigates the validity of these concerns by examining available literature and the results of a small pilot study.

Background
In May 2014 Singapore General Hospital announced a new dress policy for all staff. Hanging lanyards were banned and replaced with retractable identification card holders. Dr Ling Moi Lin, the hospital’s director of infection control, explained that the hospital aimed “to ensure that ties and lanyards do not flap around when staff examine patients, these objects can easily collect germs and bacteria – we do not want to carry them to other patients.” [1]
This hospital is not alone on their stance against hanging lanyards. The British National Health Service (NHS) Standard Infection Prevention and Control guidelines published in March 2013 lists wearing neckties or lanyards during direct patient care as “bad practice”. The guidelines state that lanyards “come into contact with patients, are rarely laundered and play no part in patient care”. [2] Closer to home the current 2013 Bare Below the Elbows campaign, a Queensland Government initiative aiming to improve the effectiveness of hand hygiene performed by health care workers, recommends that retractable (or similar) identification card holders are used in place of lanyards. [3] Other Australian states and many individual hospitals have adopted similar recommendations. [4,5]
However, some hospitals and medical schools continue to require staff and students to wear lanyards. For example James Cook University medical students are provided with one lanyard, which must be worn in all clinical settings (whether that be at the medical school during clinical skills sessions or at the hospital) for the entire duration of their six-year degree. [6] The University of Queensland 2013 medical student guide for their Sunshine Coast clinical school states that students must wear their lanyards and display identification badges at all times in teaching locations. [7] This is not concordant with the current Queensland Government initiative recommendations.
The NHS Standard Infection Prevention and Control guidelines are also being breached by medical schools requiring their students to wear lanyards. London Global University states that lanyards are important in that they remind patients who students are and clinical teachers and other professionals that they are in a teaching hospital. However students are required to use a safety pin to attach the end of their lanyard to fixed clothing. [8] A similar policy is in place in Cardiff University where students must wear lanyards but ensure that they are not “dangling” freely when carrying out examinations and procedures. [9] So how harmful could the humble, dangling lanyard really be?
How harmful could the lanyard be?
Each year there are around 200,000 healthcare-associated infections in Australian acute healthcare facilities. Nosocomial infections are the most common complication affecting patients in hospital. These potentially preventable adverse effects cause unnecessary pain and suffering for patients and their families, prolong hospital stays and are costly to the health care system. [10]
Improving hand hygiene among healthcare workers is currently the single most effective intervention to reduce the risk of nosocomial infections in Australian hospitals. [11] The World Health Organisation guidelines on Hand Hygiene in Health Care indicate five moments when the hands must be washed. Two of these are before and after contact with a patient. [12]
In between these two crucial hand washes several objects are frequently touched by health care staff. Objects such as a doctor’s neckties [13-17], stethoscopes [18-20] and pens [21,22] have all been shown to carry pathogenic bacteria. The bacteria isolated include methicillin resistant Staphylococcus aureus (MRSA), found on doctors’ ties [14,16] and stethoscopes. [19] Making contact with these objects during an examination can result in the indirect transmission of microorganisms, transferring the infectious agents to a susceptible host via an intermediate object termed a fomite.
The infectious agents must be transferred from the fomites to the hands of the health care practitioners before they can be spread to patients. The efficiency of transfer of a pathogen on a surface to a practitioner’s hand after a single contact was tested by a recent study published in 2013. It isolated five known nosocomial pathogens and placed them on non-porous surfaces; after 10 seconds of contact time between a finger and the surface under a known pressure the microorganism transferred to the finger was examined. It showed that under relative humidity non-porous surfaces had a transfer efficiency of up to 79.5%. [23] This study indicates that after one contact with a contaminated fomite there is a significant transfer of microorganisms to the hands, these can then be transferred to patients.
Furthermore, if no regular preventative disinfection is performed the most common nosocomial pathogens may survive or persist on inanimate surfaces for months and can therefore be a continuous source of transmission. [24] One study conducted in the United Kingdom in 2008 approached 100 hospital staff randomly and asked them to state the frequency and method by which their lanyards were washed or decontaminated. Only 27% had ever washed their lanyards and 35% of lanyards appeared noticeably soiled. [25] This suggests that the lanyards, which doctors carry with them daily, could potentially harbour acquired infectious agents for an extended periods of time.
Two recent studies have shown that lanyards do carry pathogenic bacteria. [25,26] An Australian study by Kotsanas et al. tested lanyards and identification cards for pathogenic bacteria and found that 38% of lanyards harboured these. Nearly 10% of lanyards grew MRSA, and other pathogens found included methicillin sensitive Staphylococcus aureus, enterococci and Gram-negative bacilli. The bacterial load on lanyards was 10 times greater per unit surface area than the identification cards themselves. [26]
It has been suggested that contaminated fomites are a result of poor hand hygiene. As such it is assumed that with good hand hygiene practices wearing these objects is acceptable. It has been widely reported that nurses have far better hand hygiene habits than doctors. A recent Australian study conducted in 82 hospitals reports that nurses consistently have significantly higher levels of hand hygiene compliance. [27] If the fomite pathogenic carriage is dependent on hand hygiene then one might expect that lanyards worn by nurses would have lower pathogenic carriage. However Kotsanas et al. showed that although there was a difference in organism composition there was no significant difference between total median bacterial counts isolated from nurses’ and doctors’ lanyards. [26] This suggests that the carriage of pathogens on lanyards is not solely dependent on compliance with hand hygiene protocols.
Lanyards have thus been shown to carry bacteria, which may remain on them for months, regardless of hand hygiene practices, and have high rates of transfer to the hands of practitioners. However there have been no studies conducted to directly show that their use results in the increased transmission of bacteria. There are however some studies which have shown bacterial transfer from neckties to patients. Lanyards are similar to neckties in that they have been shown to carry pathogenic bacteria, are made of a textile material which is rarely laundered, are positioned at the waistline, have a nature to swing and inadvertently touch patients or the practitioner’s cleansed hands and have no direct role in patient care. [13-17]
A study in Pakistan found that the bacteria collected from the lower part of neckties worn by physicians correlated with bacteria isolated from their patients’ wounds after surgical review. [17] This suggests that bacterial transmission occurred. More convincingly, a recent study by Weber et al. tested the transmission of bacteria, to dummies, from doctors wearing different combinations of clothing inoculated with comparable levels of bacteria to those previously reported. After a brief 2.5-minute history and exam, cultures were obtained from the dummies at three sites. The number of contaminated mock patients was six times higher and total colony units cultured was 26 times higher when the examiner was wearing an unsecured necktie. [28] This showed that unsecured neckties do result in greater transmission of bacteria from doctors to patients. The ties may swing to directly transmit bacteria to the patient or to the cleansed hands of the doctor, which are then transferred to the patient. Lanyards would likely pose a similar risk.
In my clinical experience, unlike ties, lanyards are often inadvertently touched and fiddled with by medical students and doctors during the clinical examination of a patient. This can recontaminate hands with pathogens even after hand-washing procedures have been followed. Thus, because of this additional contact, lanyards potentially have a higher rate of bacterial transmission than neckties.
What did my pilot study show?
To test this theory I conducted a small observational study, in which 20 James Cook University fourth-year medical students were observed during the focused examination of a volunteer, posing as a patient in an imitated hospital bed setting. Twelve students conducted a focused head and neck examination whilst eight conducted an abdominal examination. The students were unaware of the nature of the study. All students observed washed their hands prior to and at the end of each clinical examination. I observed the students from when they washed their hands prior to the physical exam until their last physical contact with the patient. The mean time taken was 12 minutes. During this period two things were noted: the number of times that their hands made contact with their lanyards and the number of times that the lanyard made contact with the patient. 70% of the students’ lanyards touched their patient during the exam at least once; the mean number of times was 2.65 (SD = 2.99). 95% of students touched their lanyards during the exam; the mean number of times was 7.35 (SD = 5.28).
Many made contact with their lanyard as part of their introduction to the patient, holding their lanyard to “show” that they are in fact a medical student. Some held the lanyards to their abdomen with one hand whilst examining the patient with the other hand to prevent it making contact with the patient. Others fiddled with the lanyard whilst talking to the patient. During hand gestures, the lanyards often collided with the student’s hands and the students’ stethoscopes, prominently displayed around their necks, were often entangled with their lanyards. The amount of contact was to the extent that some students default position was standing with their hands holding their lanyards. After each forced hand movement their hands were returned to holding their lanyards.
It is also interesting to note that several students had attached objects such as pens, USBs and keypads to their lanyards. The attachment of additional objects had a slightly increased correlation with the amount of times that their hands made contact with the lanyard but almost doubled the times the lanyard made contact with the patient (2.65 to 4.67).
One student had a lanyard clip which fastened the end of his lanyard to his shirt. This student did not touch his lanyard once during the exam and his lanyard also did not make contact with the patient. There may thus be some benefit in following the lead of London Global University and Cardiff University in enforcing the use of lanyard clips or safety pins to prevent their students’ lanyards from dangling. [8,9]
This observational study adds another dimension to the argument against wearing lanyards. Like neckties, lanyards have been shown to carry pathogenic bacteria, swing to make contact with the patient, are rarely laundered, and have no direct part in patient care. This small observational study confirmed my assumption that lanyards also come into contact with examiners’ hands a significant number of times during an examination.
Role models
During the influential years at some medical schools, it is standard policy that students are required to wear a hanging lanyard even though there is a growing body of evidence which indicates that hanging lanyards should not be worn. These students can only dream of the day when their blue medical student lanyards are replaced with the lanyards with “DOCTOR” repeatedly printed. Our role models are wearing improved, larger, better lanyards. It has been proposed that advocating the presentation of up-to-date evidence based information with an emphasis on role modelling should be made an educational priority to improve hand hygiene rates. [29] Research has indicated that targeting medical students may be an effective approach to raising the low compliance rates of hand hygiene procedures of doctors. [29] Clearly advocating the role that fomites like lanyards play in the spread of nosocomial infections has not been made an educational priority and may be part of the reason why compliance with current health hygiene policies regarding their use are low.
It seems contradictory that if I do not to wash my hands at the start of a clinical examination I will fail but I could, like one student in the observation study did, touch an object shown to carry pathogenic bacteria, which I am required to wear, 23 times and still pass. Making contact with an object shown to carry pathogenic bacteria more than once per minute of clinical examination is alarming and arguably diminishes the purpose of rigorous hand washing procedures.
Conclusion
Lanyards are an easy way to carry identification cards that identify who’s who in a fast paced environment. However there is a growing body of evidence that indicates that they may be the harbour for the indirect transmission of infectious agents to patients. Several health hygiene policies have been updated to encourage health professionals not to wear lanyards during direct patient care. Some medical schools have not followed these guidelines and still require students to wear lanyards. While there is no definitive link showing the transmission of an acquired infection from the tip of a medical student’s lanyard, there is very reasonable circumstantial evidence indicating that this could easily happen. Obeying current state infection prevention guidelines and swapping hanging lanyards for retractable identification cards or simply preventing them from dangling may be useful in reducing nosocomial infections in Australia. It is about time that the lanyard is retired as a symbolic but potentially harmful relic of the past.
Acknowledgements
James Cook University clinical staff and fourth year medical students for allowing me to observe their clinical skills assessment.
Conflict of interest
None declared.
Correspondence
E de Jager: elzerie.dejager@my.jcu.edu.au
References
[1] Cheong K. SGH staff roll up their sleeves – under new dress code for better hygiene. The Straits Times [Internet]. 2014 May 16 [cited 2014 Jun 25]. Available from: www.straitstimes.com/news/singapore/health/story/sgh-staff-roll-their-sleeves-under-new- dress-code-better-hygiene-2014050
[2] NHS: National Health Service. CG1 Standard infection prevention and control guidelines [Internet]. 2014 Mar [cited 2014 Jun 25]. Available from: http://www.nhsprofessionals. nhs.uk/download/comms/cg1%20standard%20infection%20prevention%20and%20 control%20guidelines%20v4%20march%202013.pdf
[3] Queensland Government Department of Health. Bare below the elbows [Internet]. 2013 Sep [cited 2014 Jun 24]. Available from: http://www.health.qld.gov.au/chrisp/hand_hygiene/fsheet_BBE.pdf
[4] Tasmanian Government Department of Health and Human Services. Hand hygiene policy [Internet]. 2013 Apr 1[cited 2014 Jun 24] Available from: http://www.dhhs.tas.gov.au/data/assets/pdf_file/0006/72393/Hand_Hygiene_Policy_2010.pdf
[5] Australian Capital Territory Government Health. Standard operating procedure 1, hand hygiene [Internet]. 2014 March [cited 2014 June 24]. Available from: http://health.act.gov.au/c/health?a=dlpubpoldoc&document=2723
[6] James Cook University School of Medicine. Medicine student lanyards [Internet]. 2014 [cited 2014 June 24] Available from: https://learnjcu.jcu.edu.au/
[7] The University of Queensland Sunshine Coast Clinical School. 2013 Medical student guide [Internet]. 2013 [cited 2014 July 5]. Available from: https://my.som.uq.edu.au/mc/media/25223/sccs%20medical%20student%20guide%202013.pdf
[8] University College London Medical School. Policies and regulations, identity cards and name badges [Internet]. 2014 [cited 2014 July 5]. Available from: http://www.ucl.ac.uk/medicalschool/staff-students/general-information/a-z/#dress
[9] Cardiff University School of Medicine. Personal presentation [Internet]. 2013 August 22 [cited 2014 July 5]. Available from: http://medicine.cf.ac.uk/media/filer_public/2013/08/22/perspres.pdf. Published August 22, 2013
[10] Australian Government National Health and Medical Research Council. Australianguidelines for the prevention and control of infection in healthcare [Internet]. 2010 [cited2014 June 24]. Available from: http://www.nhmrc.gov.au/book/australian-guidelines-prevention-and-control-infection-healthcare-2010/introduction
[11] Australian Commission on Safety and Quality in Healthcare Hand Hygiene Australia. 5 Moments for hand hygiene [Internet]. 2009 [cited 2014 July 7]. Available from: http://www.hha.org.au/UserFiles/file/Manual/ManualJuly2009v2(Nov09).pdf
[12] World Health Organisation. WHO guidelines on hand hygiene in health care [Internet]. Geneva. 2009 [cited 2014 July 7]. Available from: http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf
[13] Dixon M. Neck ties as vectors for nosocomial infection. ICM. 2000;26(2):250.
[14] Ditchburn I. Should doctors wear ties? J Hosp Infect. 2006;63(2):227-8.
[15] Lopez PJ, Ron O, Parthasarathy P, Soothill J, Spitz L. Bacterial counts from hospital doctors’ ties are higher than those from shirts. Am J Infect Control. 2009; 37(1):79-80.
[16] Bhattacharya S. Doctors’ ties harbour disease- causing germs. NewScientist.com [Internet]. 2004 May 24 [cited 2014 June 20]. Available from: http://www.newscientist. com/arti- cle/dn5029-doctors-ties-harbour-diseasecaus- ing-germs.html
[17] Shabbir M, Ahmed I, Iqbal A, Najam M. Incidence of necktie as a vector in nosocomial infection. Pak J Surg. 2013; 29(3):224-225.
[18] Marinella MA, Pierson C, Chenoweth C. The stethoscope. A potential source of nosocomial infection? Arch Intern Med. 1997;157(7):786-90.
[19] Madar R, Novakova E, Baska T. The role of non-critical health-care tools in the transmission of nosocomial infections. Bratisl Med J. 2005;106(11):348-50.
[20] Lokkur PP, Nagaraj S. The prevalence of bacterial contamination of stethoscope diaphragms: a cross sectional study, among health care workers of a tertiary care hospital. Indian I Med Microbiol. 2014;32(2):201-2.
[21] French G, Rayner D, Branson M, Walsh M. Contamination of doctors’ and nurses’ pens with nosocomial pathogens. Lancet. 1998;351(9097):213.
[22] Datz C, Jungwirth A, Dusch H, Galvan G, Weiger T. What’s on doctors’ ball point pens? Lancet. 1997;350(9094):1824.
[23] Lopez GU, Gerba CP, Tamimi AH, Kitajima M, Maxwell SL, Rose JB. Transfer efficiency of bacteria and viruses from porous and nonporous fomites to fingers under different relative humidity conditions. Appl Environ Microbiol. 2013;79(18):5728-34.
[24] Kramer A, Schwebke I, Kampf G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect Dis. 2006;6:130.
[25] Alexander R, Volpe NG, Catchpole C, Allen R, Cope S. Are lanyards a risk for nosocomialtransmission of potentially pathogenic bacteria? J Hosp Infect. 2008;70(1):92-3.
[26] Kotsanas D, Scott C, Gillespie EE, Korman TM, Stuart RL. What’s hanging around your neck? Pathogenic bacteria on identity badges and lanyards. Med J Aust. 2008;188(1):5-8.
[27] Azim S, McLaws ML. Doctor, do you have a moment? National Hand Hygiene Initiative compliance in Australian hospitals. Med J Aust. 2014;200(9):534-7.
[28] Weber RL, Khan PD, Fader RC, Weber RA. Prospective study on the effect of shirt sleeves and ties on the transmission of bacteria to patients. J Hosp Infect. 2012;80(3):252-4.
[29] Hall L, Keane L, Mayoh S, Olesen D. Changing learning to improve practice – Handhygiene education in Queensland medical schools. Healthcare Infection. 2010 Dec;15(4):126-129.


 Skin forms a dynamic interface with the external environment and is a complex organisation of cell types and associated structures that performs many essential functions. Although the stratum corneum of full-term neonates is analogous to that of adult skin, structural and compositional differences of the skin renders the newborn more susceptible to bacterial colonisation. Particularly for the preterm neonate, impaired cutaneous barrier function and an immature immune system reduce the capacity to defend against bacterial pathogens. The majority of cutaneous bacterial infections are localised to the skin and are easily treated, however, systemic bacterial infection and disseminated disease in the neonatal period may be life-threatening.
Skin forms a dynamic interface with the external environment and is a complex organisation of cell types and associated structures that performs many essential functions. Although the stratum corneum of full-term neonates is analogous to that of adult skin, structural and compositional differences of the skin renders the newborn more susceptible to bacterial colonisation. Particularly for the preterm neonate, impaired cutaneous barrier function and an immature immune system reduce the capacity to defend against bacterial pathogens. The majority of cutaneous bacterial infections are localised to the skin and are easily treated, however, systemic bacterial infection and disseminated disease in the neonatal period may be life-threatening.![Table 1. Differences between newborn and adult skin. [1,2]](https://www.amsj.org/wp-content/uploads/2015/04/v5_i1_a22_1-300x261.jpg)


 Anaesthesia is a relatively new field in modern medicine. Prior to its development, most surgical procedures were either minor or emergency operations. [1] It is clear that modern surgery and the considerable benefits it brings would be impossible without the significant academic, pharmacological, and practical advances in anaesthesia during the 19th and 20th centuries. First and foremost among these is the development of safe and effective general anaesthesia.
Anaesthesia is a relatively new field in modern medicine. Prior to its development, most surgical procedures were either minor or emergency operations. [1] It is clear that modern surgery and the considerable benefits it brings would be impossible without the significant academic, pharmacological, and practical advances in anaesthesia during the 19th and 20th centuries. First and foremost among these is the development of safe and effective general anaesthesia.
 A 27-year-old male is referred to a sexual health clinic by a general practitioner (GP). He presents with a widespread maculopapular rash, fever and malaise for the past four days. Whilst he does not describe any other symptoms, he did notice a painless genital ulcer approximately four weeks ago. The ulcer resolved spontaneously; hence he initially did not seek medical advice. He does not have a stable sexual partner and mentions engaging in several episodes of unprotected sex with both women and men in the previous three months. Secondary syphilis is the suspected diagnosis given the widespread rash and preceding chancre, and testing confirms this with a positive syphilis enzyme-linked immunoassay (EIA) screening test, Treponema pallidum particle agglutination assay (TPPA), and an rapid plasma reagin (RPR) of 1:32. As part of a sexual health screen, he tested positive for rectal gonorrhoea by culture. The treatment regime includes 1.8 g intramuscular benzathine penicillin for syphilis, in addition to 500 mg intramuscular ceftriaxone and 1g oral azithromycin for gonorrhoea, all given as stat doses. Before signing the drug order, the clinician questions about any allergies. The patient mentions having an allergic reaction to penicillin when he was six years old but cannot remember any particular details. What is the plan now?
A 27-year-old male is referred to a sexual health clinic by a general practitioner (GP). He presents with a widespread maculopapular rash, fever and malaise for the past four days. Whilst he does not describe any other symptoms, he did notice a painless genital ulcer approximately four weeks ago. The ulcer resolved spontaneously; hence he initially did not seek medical advice. He does not have a stable sexual partner and mentions engaging in several episodes of unprotected sex with both women and men in the previous three months. Secondary syphilis is the suspected diagnosis given the widespread rash and preceding chancre, and testing confirms this with a positive syphilis enzyme-linked immunoassay (EIA) screening test, Treponema pallidum particle agglutination assay (TPPA), and an rapid plasma reagin (RPR) of 1:32. As part of a sexual health screen, he tested positive for rectal gonorrhoea by culture. The treatment regime includes 1.8 g intramuscular benzathine penicillin for syphilis, in addition to 500 mg intramuscular ceftriaxone and 1g oral azithromycin for gonorrhoea, all given as stat doses. Before signing the drug order, the clinician questions about any allergies. The patient mentions having an allergic reaction to penicillin when he was six years old but cannot remember any particular details. What is the plan now?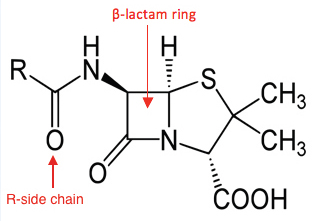

 Structured physical activity has a wide range of health benefits that include the prevention of chronic diseases such as cancer, cardiovascular disease, diabetes and obesity. [1] There is also consensus that exercise has a short-term ‘feel good’ effect that improves mood and wellbeing. [2-4] Recently, converging interest in these two areas has spawned an explosion of research aimed at treating diseases such as depression using nothing more than exercise. [5-7] A 2012 meta-analysis of over 25 trials found that prescribing exercise to treat depression is on par with pharmacological and physiological interventions, and that exercise alone is moderately more effective than no therapy. [8] The study also highlights that prescribing exercise for depression is not straightforward. Poor patient attendance rates, along with issues including exercise adherence and the type, duration and intensity of exercise, all question whether prescribing exercise for sufferers of depression is indeed appropriate. The authors of the study admit the implementation is complex and that further study is required. Nonetheless, is there a role for medical students in encouraging physical activity as treatment? Can our skills in motivational interviewing and goal setting play a role? If we re-examine the use of exercise from a patient-centred perspective, medical students can promote exercise adherence and support those who are already exercising to stay exercising. In doing so, we can facilitate the prescription of exercise and possibly prevent depression. [5,7,9]
Structured physical activity has a wide range of health benefits that include the prevention of chronic diseases such as cancer, cardiovascular disease, diabetes and obesity. [1] There is also consensus that exercise has a short-term ‘feel good’ effect that improves mood and wellbeing. [2-4] Recently, converging interest in these two areas has spawned an explosion of research aimed at treating diseases such as depression using nothing more than exercise. [5-7] A 2012 meta-analysis of over 25 trials found that prescribing exercise to treat depression is on par with pharmacological and physiological interventions, and that exercise alone is moderately more effective than no therapy. [8] The study also highlights that prescribing exercise for depression is not straightforward. Poor patient attendance rates, along with issues including exercise adherence and the type, duration and intensity of exercise, all question whether prescribing exercise for sufferers of depression is indeed appropriate. The authors of the study admit the implementation is complex and that further study is required. Nonetheless, is there a role for medical students in encouraging physical activity as treatment? Can our skills in motivational interviewing and goal setting play a role? If we re-examine the use of exercise from a patient-centred perspective, medical students can promote exercise adherence and support those who are already exercising to stay exercising. In doing so, we can facilitate the prescription of exercise and possibly prevent depression. [5,7,9]