A fit 40-year-old man presented to hospital with signs and symptoms consistent with a large anterior stroke. He underwent intravenous thrombolysis and later developed cerebral oedema, which was managed with a decompressive hemicraniectomy. Investigation findings revealed the patient had tight mitral stenosis most likely due to rheumatic heart disease. The report discusses the pathogenesis of stroke due to rheumatic heart disease and compares the use of intravenous thrombolysis and mechanical thrombectomy in the treatment of ischaemic stroke.
Introduction
Cerebrovascular disease is the second leading cause of death and the leading cause of disability in Australia [1]. This case report describes a 40-year-old who presented with symptoms consistent with a large anterior stroke. The report illustrates the causes of stroke in a young person, and outlines the pathogenesis of stroke due to rheumatic heart disease. It also highlights the serious complication of cytotoxic and ionic cerebral oedema that can occur after a large stroke, and the use of hemicranectomy in its management. The case report also discusses and compares the use of intravenous thrombolysis and mechanical thrombectomy in the treatment of ischaemic stroke.
Case Description
A 40-year-old man collapsed at home and was transported by ambulance to the emergency department (ED) of a regional hospital. En route to the hospital he was confused and was noted to have left sided weakness and facial droop. He emigrated from India at age 13, had no known medical conditions, and was on no regular medications. There was no family history of stroke or any prothrombotic conditions. He reportedly did not smoke or drink alcohol, he exercised regularly, and was not overweight.
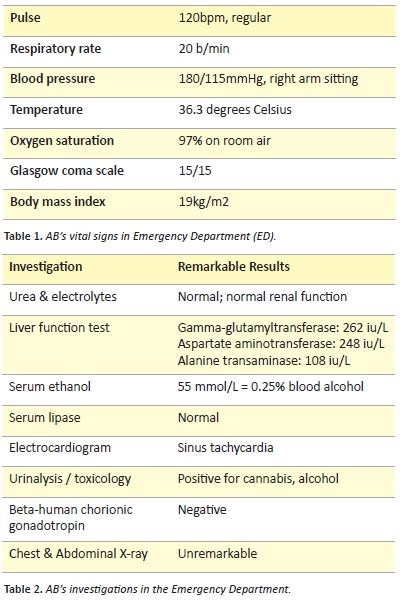
On examination in the ED, he had a Glasgow Coma Score (GCS) of 13, left-sided facial droop, dysarthria, complete flaccid paralysis of the left upper limb, and left lower limb weakness (unable to resist gravity). He was assessed as having a National Institute of Health Stroke Score (NIHSS) of 14. On auscultation, his chest was clear and heart sounds were reported as being dual with no murmurs. An ECG was performed, which showed he was in sinus rhythm. A computerised tomography (CT) brain scan showed an area of hypodense brain tissue corresponding to the right middle cerebral artery (MCA) territory and a dense right MCA sign, representing increased attenuation of the proximal portion of the MCA (Figure 1). There were no signs of acute haemorrhage on the CT scan. A CT angiogram was not performed. These findings were consistent with a large right MCA ischaemic stroke. Since all inclusion criteria were met with no contraindications to therapy, the patient was treated with alteplase within four hours of symptom onset. The patient was observed for signs of bleeding; and vital signs, cardiac rhythm, blood glucose, and neurological function were checked regularly following alteplase administration. Approximately three hours later, the patient’s GCS dropped to 11. A CT brain scan was repeated, which showed further development of cerebral oedema and effacement of the sylvian fissure, but no acute haemorrhage. Due to his neurological deterioration and worsening cerebral oedema, he was transferred to a tertiary hospital to undergo a decompressive hemicraniectomy.

Figure 1: A non-contrast CT scan of the brain showing a dense right middle cerebral artery sign [32].
On examination in the intensive care unit, post-hemicraniectomy, the patient’s neurological function had improved to a GCS of 14. He still had a dense left hemiparesis, reduced left sided sensation, facial droop, dysarthria, and left-sided neglect. The intensivist identified a diastolic murmur with an opening snap that had not been picked up on previous examinations. The patient was extensively investigated to find the cause of the stroke. This included a full blood count (FBC); urea, electrolytes, and creatinine (UEC); coagulation studies; fasting lipids and glucose; ESR and CRP; syphilis serology; vasculitis screen; prothrombotic screen; chest x-ray; ECG; and carotid artery doppler scan. These results were all normal. An echocardiogram showed tight mitral stenosis (MS) with a mitral valve area of 1.8 cm2, thickened and restricted valve leaflets, and a large dilated left atrium measuring 49 mm. The systolic pulmonary artery pressure was also measured during echocardiogram which demonstrated no significant pulmonary hypertension.
It was hypothesised by the intensivist that the stroke resulted from a thrombus forming in the large, dilated, left atrium due to paroxysmal atrial fibrillation (AF) caused by the MS. Even though no significant childhood illness was reported by the patient or his family, the MS was believed to be the result of rheumatic heart disease (RHD) based on his echocardiogram findings and the patient’s emigration history.
The patient was reviewed by cardiology and was commenced on warfarin with a target INR of between two to three. It was also recommended that he receive intramuscular penicillin injections of 900 mg monthly for the secondary prevention of RHD. A follow-up echocardiogram and cardiology appointment was booked for six weeks’ time to determine whether a percutaneous balloon mitral valvuloplasty would be indicated to treat his MS. A follow up neurosurgery appointment was also planned for discussion of a future cranioplasty. Once stable, the patient was transferred to a rehabilitation facility to undergo an intensive multi-disciplinary program consisting of physiotherapy, speech therapy, and occupational therapy with the aim of maximising his physical, psychological, social, and financial independence.
Discussion
Young patients with minimal risk factors who have suffered a stroke require more extensive investigations in order to find an underlying cause. Conditions associated with ischaemic stroke in young adults include cardiac abnormalities, premature atherosclerosis, hypertension, vasculopathy including arterial dissection, recent pregnancy, other hypercoagulable states, smoking, illicit drug use, metabolic disorders, and migraine with aura [2]. A meta-analysis by Schurks et al. [3] found migraine with aura to be an independent risk factor for developing ischaemic stroke, but the absolute increase in the risk of stroke was found to be small. The pathophysiology underlying migraine as a possible cause of stroke is not yet clear [3]. Several metabolic conditions are also associated with acute ischaemic stroke in young adults. Cerebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is a metabolic condition which leads to progressive degeneration of smooth muscle cells in the vessel wall [4]. Patients with CADASIL may present with migraine, transient ischaemic attack, or ischaemic stroke in late childhood or early adulthood [4]. Mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes (MELAS) is another metabolic condition that causes stroke-like episodes in young adults, leading to progressive neurologic dysfunction and dementia. The hallmarks of this syndrome are episodes of hemiparesis, hemianopia, or cortical blindness [5]. Cardiac defects such as patent foramen ovale (PFO) and atrial septal defect (ASD) have also been implicated in the pathogenesis of stroke in younger adults [6]. The mechanism is via an embolus that originates in the systemic venous circulation and enters the systemic arterial circulation through the cardiac defect. Emboli can originate from the lower extremity or pelvic veins, tricuspid vegetations, or right atrial thrombi [6]. Many of these conditions only account for a very small percentage of stroke in young adults. A large cohort study by Putaaya et al. [7] looked at patients aged 15-49 with their first ever ischaemic stroke. They found the most common aetiologies were cardioembolism and cervicocephalic atrial dissection.
Atrial fibrillation is a common causes of cardioembolic stroke, with around 25% of ischaemic stroke patients in Australia having AF [8]. Coronary artery disease, hypertension, heart failure, and valvular heart disease are the most common causes of AF [9]. In this case report the patient’s thrombus was hypothesised to have been caused by paroxysmal AF due to rheumatic MS. Rheumatic heart disease is a result of cardiac inflammation and scarring triggered by an autoimmune reaction to infection with group A streptococci [10]. This can result in thickened and restricted valve leaflets, leading to valve stenosis and/or regurgitation [10]. Rheumatic heart disease is the most common cause of MS [11]. One of the most common complications of rheumatic MS is AF [12]. In rheumatic MS, AF may initially be paroxysmal, but eventually it becomes chronic as the MS and left atrial dilatation progress [11]. AF may cause systemic embolism from mural thrombus development in the left atrium leading to stroke. Patients with MS and AF should therefore receive long-term prophylactic anticoagulation. Left atrial thrombus can occur in MS, even when sinus rhythm is present. This is due to left atrial dilatation, low blood velocity, and disorganised blood flow. Therefore, prophylactic anticoagulation should also be considered for patients with MS and a dilated left atrium even if in sinus rhythm [12]. The 2014 American Heart Association (AHA) guidelines on management of valvular heart disease recommends the use of warfarin in patients with MS and at least one of the following conditions: paroxysmal AF, permanent AF, prior embolic event, or proven left atrial thrombus [13]. Newer oral anticoagulants are now approved for the prevention of systemic embolism in adults with non-valvular AF. However, they are not approved for use in patients with MS, as this patient group was excluded in clinical trials [13].
Another treatment option for MS is percutaneous balloon mitral valvuloplasty. This procedure involves a balloon catheter being inserted via the femoral vein and placed in the left atrium. The balloon is positioned across the stenotic mitral valve and inflated, thereby separating the stenotic leaflets along the commissures. The criteria for percutaneous balloon mitral valvuloplasty in an asymptomatic patient with MS is a mitral valve area ≤1.0 cm2, favorable valve morphology, absence of moderate to severe mitral regurgitation, and no left atrial thrombus [13]. The patient in this case report did not meet the AHA criteria and therefore is unlikely to undergo valvuloplasty. In asymptomatic patients with MS, follow-up echocardiography is recommended every three to five years, if the mitral valve area is >1.5 cm2 [13]. The patient in this case report should therefore undergo regular echocardiograms to monitor the progression of his MS.
One of the serious complications of a large MCA stroke is the development of cytotoxic and ionic cerebral oedema. Cerebral oedema is the result of cells being unable to maintain ATP-dependent Na+/K+ membrane pumps which are responsible for a high extracellular and low intracellular Na+ concentration [14]. When energy falls due to cerebral ischaemia, these pumps cease to operate and Na+ accumulates in the cell, drawing with it Cl– and water along an osmotic gradient [14]. Space-occupying cerebral oedema can elevate intracranial pressure and lead to brain herniation [15]. The development of space-occupying cerebral oedema due to a large infarction leads to neurologic deterioration with signs that typically include decreased arousal, pupillary changes, and worsening of motor responses [16]. These neurological signs are indicators of the need to intervene urgently. Decompressive hemicraniectomy and durotomy is a surgical technique used to relieve the increased intracranial pressure and brain tissue shifts that occur in the setting of large cerebral hemisphere space-occupying lesions. The technique involves removal of bone tissue and incision of the restrictive dura mater covering the brain, allowing swollen brain tissue to herniate upwards through the surgical defect rather than downwards to compress the brainstem [16]. In patients with malignant MCA infarction, decompressive surgery undertaken within 48 hours of stroke onset reduces mortality and increases the number of patients with a favorable functional outcome [17].
The immediate aim in the management of acute ischaemic stroke is to recanalise the occluded vessel as quickly, safely, and effectively as possible to restore blood supply to the ischaemic brain region [18]. Thrombolytic therapy is an effective strategy for salvaging ischaemic brain tissue that is not already infarcted following ischaemic stroke [19]. However, there is a risk of haemorrhage, a narrow window during which it can be administered, and multiple contraindications to its use [18]. The indications for administering thrombolysis include the onset of ischaemic stroke within the preceding four-and–a-half hours in Australia and Europe, and within three hours in the United States. There must also be no signs of haemorrhage on the brain CT scan [18]. Where available, assessment of ischaemic brain injury with either diffusion and perfusion MRI or with perfusion CT should be performed if the findings are likely to influence treatment decisions. However, these should be used rather than CT only if it does not delay treatment with intravenous alteplase [20]. A 2014 meta-analysis by Emberson et al. [21] evaluated individual patient data from 6756 subjects who were allocated to intravenous alteplase or control within three to six hours of acute ischaemic stroke onset. The primary outcome measure was the proportion of patients achieving a good stroke outcome at three or six months as defined by a modified Rankin scale score. The modified Rankin scale measures the degree of disability or dependence in the patient’s daily activities [21]. The results of Emberson’s analysis showed that the sooner intravenous alteplase treatment is initiated, the more likely it is to be beneficial, and that the benefit extends to treatment started within four-and-a-half hours of stroke onset [21]. It was found that beyond five hours, harm may exceed benefit as alteplase increased the risk of symptomatic intracranial haemorrhage (6.8% vs 1.3% control) and fatal intracranial haemorrhage within seven days (2.7% vs 0.4% control) [21]. A recent systematic review by Wardlaw et al. [22] found similar results, that treatment with intravenous alteplase within three hours of stroke was substantially more effective in reducing death or dependency than therapy given up to six hours after stroke onset.
Intra-arterial mechanical thrombectomy is another treatment option for patients with ischaemic stroke. Five large randomised control trials [23-27] demonstrated that early intra-arterial treatment using mechanical thrombectomy devices is superior to standard treatment with intravenous thrombolysis alone for large proximal vessel ischaemic stroke in the anterior circulation. The inclusion criteria for mechanical thrombectomy include a CT brain scan ruling out intracranial haemorrhage, angiography demonstrating a proximal large artery occlusion in the anterior circulation, and thrombectomy initiated within six hours of stroke onset [23]. One problem that limits the widespread clinical use of mechanical thrombectomy is that only an estimated ten percent of patients with acute ischaemic stroke have a proximal large artery occlusion in the anterior circulation and present early enough to qualify for mechanical thrombectomy [18]. Another issue that limits its widespread use is that it is restricted to major stroke centres that have specialist interventional radiology resources and expertise able to perform the procedure [18]. The Queensland Health Policy Advisory Committee on Technology published a report in December 2015 that looked at mechanical thrombolysis for ischaemic stroke [29]. They found that mechanical thrombectomy can only be safely performed in experienced centres with appropriate support in terms of imaging and multidisciplinary care, and that only large tertiary centres with stroke units are able to provide this service. They noted that this may have implications for patients who are not near to these services, especially given the time frame within which the procedure can be performed. This has implications for accessibility for rural and remote patients, and associated costs if transferring patients to tertiary centers is required [29]. Another issue is that transferring patients to tertiary centres can delay the onset of stroke treatment. However, eligible patients can receive standard treatment with intravenous alteplase if they present to hospitals where thrombectomy is not an option. Those patients with qualifying anterior circulation strokes can then be transferred to tertiary stroke centers where intra-arterial thrombectomy is available [30].
In this case report, the patient was discussed at an interventional radiology meeting at the tertiary hospital. The radiologist commented that if this patient had initially presented to the tertiary hospital rather than the regional hospital, the patient would have undergone a mechanical thrombectomy instead of, or as well as, the intravenous thrombolysis. Similar views are expressed in a 2015 editorial by neuroradiologists Pierot and Derdeyn [31]. They conclude that endovascular treatment has now been proven effective for a well-defined subset of patients with acute stroke, provided there is careful patient selection, time to reperfuse, and reperfusion rate is optimised. This illustrates that mechanical thrombectomy is now the treatment of choice for proximal, anterior, ischamic stroke if the resources and personnel are available.
Consent Declaration
Informed consent was obtained from the patient and next-of-kin for publication of this case report and accompanying figures.
Conflicts of Interest
None declared.
References
[1] Australian Institute of Health and Welfare. Stroke and its management in Australia: an update. Canberra: AIHW. 2013. Cardiovascular disease series no. 37.
[2] Ji R, Schwamm L, Pervez M, Singhal A. Ischemic stroke and transient ischemic attack in young adults: risk factors, diagnostic yield, neuroimaging, and thrombolysis. JAMA Neurol. 2013;70(1):51-57.
[3] Schürks M, Rist P, Bigal M. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ. 2009; 339:b3914.
[4] Chabriat H, Joutel A, Dichgans M, Tournier-Lasserve E, Bousser M. Cadasil. Lancet Neurol. 2009;8(7):643-53.
[5] Sproule D, Kaufmann P. Mitochondrial encephalopathy, lactic acidosis, and stroke like episodes: basic concepts, clinical phenotype, and therapeutic management of MELAS syndrome. Ann N Y Acad Sci. 2008;1142:133-58.
[6] Lamy C, Giannesini C, Zuber M, Arquizan C, Meder J, Trystram D, et al. Clinical and imaging findings in cryptogenic stroke patients with and without patent foramen ovale: the PFO-ASA Study. Atrial Septal Aneurysm. Stroke. 2002;33:706-711.
[7] Putaala J, Metso A, Metso T, Konkola N, Kraemer Y, Haapaniemi E, et al. Analysis of 1008 consecutive patients aged 15 to 49 with first-ever ischemic stroke: the Helsinki young stroke registry. Stroke. 2009;40(4)1195-203.
[8] Gattellari M, Goumas C, Aitken R, Worthington J. Outcomes for patients with ischemic stroke and atrial fibrillation. Cerebrovasc Dis. 2010;32:370–82 .
[9] Falk R. Atrial fibrillation. N Engl J Med. 2001;344:1067-78.
[10] Patrick A. Pathology of rheumatic heart disease [Internet]. Emedicine. 2013 Oct 15 [cited 2015 Aug 10]. Available from: http://emedicine.medscape.com/article/1962779-overview.
[11] National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand. Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease [internet]. Canberra: National Heart Foundation of Australia. 2012 [cited 2015 Aug 10]. 135 p. Available from: https://www.rhdaustralia.org.au/arf-rhd-guideline
[12] Keren G, Etzion T, Sherez J. Atrial fibrillation and atrial enlargement in patients with mitral stenosis. Am Heart J. 1987;114(5):1146-55.
[13] Nishimura R, Otto C, Bonow R, Carabello B, Erwin J, Guyton R, et al. AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;63(22)57-185.
[14] Simard M, Kent T, Chen M, Tarasov K, Gerzanich V. Brain oedema in focal ischaemia: molecular pathophysiology and theoretical implications. Lancet Neurol. 2007;6(3):258-68.
[15] Wijdicks E, Sheth K, Carter B, Greer D, Kasner S, Kimberly W, et al. Recommendations for the management of cerebral and cerebellar infarction with swelling: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(4):1222-38.
[16] Gupta R, Elkind M. Decompressive hemicraniectomy for malignant middle cerebral artery territory infarction, UpToDate [Internet]. 2015 Aug. [cited 2015 Aug 8]. Available from: http://www.uptodate.com/contents/decompressive-hemicraniectomy-for-malignant-middle-cerebral-artery-territory-infarction.
[17] Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2007;6(3):215-22.
[18] Samuels O, Filho J. Reperfusion therapy for acute ischemic stroke, UpToDate [Internet]. 2015 Aug. [cited 2015 Aug 8]. Available from: http://www.uptodate.com/contents/reperfusion-therapy-for-acute-ischemic-stroke.
[19] Islam M, Anderson C, Hankey G, Hardie K, Carter K, Broadhurst R, et al. Trends in incidence and outcome of stroke in Perth, Western Australia during 1989 to 2001: the Perth community stroke study. Stroke. 2008;39(3):776–82.
[20] Filho j, Neuroimaging of acute ischemic stroke, Uptodate [internet]. 2016 May. [cited 2016 June 10]. Available from: http://www.uptodate.com/contents/neuroimaging-of-acute-ischemic-stroke.
[21] Emberson J, Lees K, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929-35.
[22] Wardlaw J, Murray V, Berge E, Del Zoppo G. Thrombolysis for acute Ischemic stroke. Cochrane database syst rev [internet]. 2014;7(4). Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000213.pub3.
[23] Berkhemer O, Fransen P, Beumer D, Van den Berg L, Lingsma H, Yoo A, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11-20.
[24] Goyal M, Demchuk A, Menon B, Eesa M, Rempel J, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019-30.
[25] Saver J, Goyal M, Bonafe A, Diener H, Levy E, Pereira V, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J of Med. 2015;372(24):2285-95.
[26] Campbell B, Mitchell P, Kleinig T, Dewey H, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009-18.
[27] Jovin T, Chamorro A, Cobo E, Molina C, Rovira A, San Roman L, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296-306.
[28] Furlan A. Endovascular therapy for stroke–it’s about time. N Engl J Med 2015;372(24):2347-9.
[29] Queensland department of health policy advisory committee on technology. Endovascular clot retrieval with thrombolysis for ischemic stroke [internet]. Brisbane. Queensland department of health. 2015 Dec [cited Mar 2016]. 18 p. Available from: https://www.health.qld.gov.au/healthpact/docs/briefs/wp226-mech-thrombectomy.pdf
[30] Sheth KN, Smith EE, Grau-Sepulveda MV, Kleindorfer D, Fonarow G, Schwamm L. Drip and ship thrombolytic therapy for acute ischemic stroke: use, temporal trends, and outcomes. Stroke. 2015;46(3):732-9.
[31] Pierot L, Derdeyn C. Interventionalist perspective on the new endovascular trials. Stroke. 2015;46:1440-46.
[32] Gaillard F. A non-contrast CT scan of the brain showing a dense right middle cerebral artery sign [image on the internet]. Radiopaedia. [viewed 2016 June 10]. Available from: http://radiopaedia.org/cases/17958.