With the human genome sequenced a decade ago and the concurrent development of genomics, pharmacogenetics and proteomics, the field of personalised cancer treatment appears to be a maturing reality. It is recognised that the days of ‘one-sizefi ts-all’ and ‘trial and error’ cancer treatment are numbered, and such conventional approaches will be refined. The rationale behind personalised treatment is to target the genomic aberrations driving tumour development while reducing drug toxicity due to altered drug metabolism encoded by the patients’ genome. That said, a number of key challenges, both scientific and non-scientific, must be overcome if we are to fully exploit knowledge of cancer genomics to develop targeted therapeutics and informative biomarkers. The progress of research has yet to be translated to substantial clinical benefits, with the exception of a handful of drugs (tamoxifen, imatinib, trastuzumab). It is only recently that new targeted drugs have been integrated into the clinical armamentarium. So the question remains: Will there be a day when doctors no longer make treatment choices based on population-based statistics but rather on the specific characteristics of individuals and their tumours?
With the human genome sequenced a decade ago and the concurrent development of genomics, pharmacogenetics and proteomics, the field of personalised cancer treatment appears to be a maturing reality. It is recognised that the days of ‘one-sizefi ts-all’ and ‘trial and error’ cancer treatment are numbered, and such conventional approaches will be refined. The rationale behind personalised treatment is to target the genomic aberrations driving tumour development while reducing drug toxicity due to altered drug metabolism encoded by the patients’ genome. That said, a number of key challenges, both scientific and non-scientific, must be overcome if we are to fully exploit knowledge of cancer genomics to develop targeted therapeutics and informative biomarkers. The progress of research has yet to be translated to substantial clinical benefits, with the exception of a handful of drugs (tamoxifen, imatinib, trastuzumab). It is only recently that new targeted drugs have been integrated into the clinical armamentarium. So the question remains: Will there be a day when doctors no longer make treatment choices based on population-based statistics but rather on the specific characteristics of individuals and their tumours?
Introduction
In excess of 100,000 new cases of cancer were diagnosed in Australia in 2010, and the impact of cancer care on patients, their carers, and the Australian society is hard to ignore. Cancer care itself consumes $3.8 billion per year in Australia, constituting close to one-tenth of the annual health budget. [1] As such, alterations to our approach to cancer care will have wide-spread impacts on the health of individuals as well as on our economy. The first ‘golden era’ of cancer treatment began in the 1940s, with the discovery of the effectiveness of the alkylating agent, nitrogen mustard, against non-Hodgkin’s lymphoma. [2] Yet the landmark paper that demonstrated cancer development required more than one gene mutation was published only 25 years ago. [3] With the discovery of the human genome sequence, [4] numerous genes have been implicated in the development of cancer. Data from The Cancer Genome Atlas (TCGA) [5] and the International Cancer Genome Consortium (ICGC) [6] reveal that even within a cancer subtype, the mutations driving oncogenesis are diverse.
The more we learn about the molecular basis of carcinogenesis, the more the traditional paradigm of chemotherapy ‘cocktails’ classified by histomorphological features appears inadequate. In many instances, this classification system correlates poorly with treatment response, prognosis and clinical outcome. Patients within a given diagnostic category receive the same treatment despite biological heterogeneity, meaning that some with aggressive disease may be undertreated, and some with indolent disease may be overtreated. In addition, these generalised cytotoxic drugs have many side eff ects, a low specifi city, low concentration being delivered to tumours, and the development of resistance, which is an almost universal feature of cancer cells.
In theory, personalised treatment involves targeting the genomic aberrations driving tumour development while reducing drug toxicity due to altered drug metabolism encoded by the patient’s genome. The outgrowth of innovations in cancer biotechnology and computational science has enabled the interrogation of the cancer genome and examination of variation in germline DNA. Yet there remain many unanswered questions about the efficacy of personalised treatment and its applicability in clinical practice, which this review will address. The transition from morphology-based to a genetics-based taxonomy of cancer is an alluring revolution, but not without its challenges.
This article aims to outline the current methods in molecular profiling, explore the range of biomarkers available, examine the application of biomarkers in cancers common to Australia, such as melanoma and lung cancer, and to investigate the implications and limitations of personalised medicine in a 21st century context.
Genetic profiling of the cancer genome
We now know that individual tumour heterogeneity results from the gradual acquirement of genetic mutations and epigenetic alterations (changes in DNA expression that occur without alterations in DNA sequence). [7,8] Chromosomal deletions, rearrangements, and gene mutations are selected out during tumour development. These defects, known as ‘driver’ mutations, ultimately modify protein signalling networks and create a survival advantage for the tumour cell. [8-10] As such, pathway components vary widely among individuals leading to a variety of genetic defects between individuals with the same type of cancer.
Such heterogeneity necessitates the push for a complete catalogue of genetic perturbations involved in cancer. This need for a large-scale analysis of gene expression has been realised by current high throughput technologies such as DNA array technology. [11,12] Typically, a DNA array is comprised of multiple rows of complementary DNA (cDNA) samples lined up in dots on a small silicon chip. Today, arrays for gene expression profiling can accommodate over 30,000 cDNA samples. [13] Pattern recognition software and clustering algorithms promote the classification of tumour tissue specimens with similar repertoires of expressed genes. This has led to an explosion of genome-wide association studies (GWAS) which have identified new chromosomal regions and DNA variants. This information has been used to develop multiplexed tests that hunt for a range of possible mutations in an individual’s cancer, to assist clinical decision-making. The HapMap aims to identify the millions of single nucleotide polymorphisms (SNPs), which are single nucleotide differences in the DNA sequence, which may confer individual differences in susceptibility to disease. The HapMap has identified low-risk genes for breast, prostate and colon cancers. [14] TCGA and ICGC have begun cataloguing significant mutation events in common cancers. [5,6] OncoMap provides such an example, where alterations in multiple genes are screened by mass spectrometry. [15]
The reproduction and accuracy of microarray data needs to be addressed cautiously. ‘Noise’ from analysing thousands of genes can lead to false predictions and, as such, it is difficult to compare results across microarray studies. In addition, cancer cells alter their gene expression when extrapolated from their environment, potentially yielding misleading results. The clinical utility of microarrays is difficult to determine, given the variability of the assays themselves as well as the variability between patients and between the laboratories performing the analyses.
Types of cancer biomarkers
This shif offerrom entirely empirical cancer treatment to stratified and eventually personalised approaches requires the discovery of biomarkers and the development of assays to detect them (Table 1). With recent technological advances in molecular biology, the range of cancer biomarkers has expanded, which will aid the implementation of effective therapies into the clinical armamentarium (Figure 1). However, during the past two decades, fewer than twelve biomarker assays have been approved by the US Food and Drug Administration (FDA) for monitoring response, surveillance or the recurrence of cancer. [16]
Early detection biomarkers
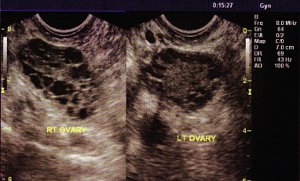
Most current methods of early cancer detection, such as mammography or cervical cytology, are based on anatomic changes in tissues or morphologic changes in cells. Various molecular markers, such as protein or genetic changes, have been proposed for early cancer detection. For example, PSA is secreted by prostate tissue and has been approved for the clinical management of prostate cancer. [17] CA-125 is recognised as an ovarian cancer-specific protein. [18]
Diagnostic biomarkers
Examples of commercial biomarker tests include the Oncotype DX biomarker test and MammaPrint test for breast cancer. Oncotype DX is designed for women newly diagnosed with oestrogen-receptor (ER) positive breast cancer which has not spread to lymph nodes. The test calculates a ‘recurrence score’ based on the expression of 21 genes. Not covered by Medicare, it will cost US$4,075 for each woman. One study found that this test persuaded oncologists to alter their treatment recommendations for 30% of their patients. [19]
Prognostic biomarkers
The tumour, node, metastasis (TNM)-staging system is the standard for prediction of survival in most solid tumours based on clinical, gross and pathologic criteria. Additional information can be provided with prognostic biomarkers, which indicate the likelihood that the tumour will return in the absence of any further treatment. For example, for patients with metastatic nonseminomatous germ cell tumours, serum-based biomarkers include α-fetoprotein, human chorionic gonadotropin, and lactate dehydrogenase.
Predictive biomarkers
Biomarkers can also prospectively predict response (or lack of response) to specific therapies. The widespread clinical usage of ER and progesterone receptors (PR) for treatment with tamoxifen, and human epidermal growth factor receptor-2 (HER-2) for treatment with trastuzumab, is evidence of the usefulness of predictive biomarkers. Epidermal growth factor receptor (EGFR) is overexpressed in multiple cancer types. EGFR mutation is a strong predictor of a favourable outcome if treated with EGFR tyrosine kinase inhibitors such as gefitinib in non-small cell lung carcinoma (NSCLC) and anti-EGFR monoclonal antibodies such as cetuximab or panitumumab in colorectal cancer. [20] Conversely, the same cancers with KRAS mutations are associated with primary resistance to EGFR tyrosine kinase inhibitors. [21,22] This demonstrates that biomarkers, such as KRAS mutation status, can predict which patient may or may not benefit from anti-EGFR therapy (Figure 2).
Pharmacodynamic biomarkers
Determining the correct dosage for the majority of traditional chemotherapeutic agents presents a challenge because most drugs have a narrow therapeutic index. Pharmacodynamic biomarkers, in theory, can be used to guide dose selection. The magnitude of BCR–ABL kinase activity inhibition was found to correlate with clinical outcome, possibly justifying the personalised selection of drug dose. [23]
The role of biomarkers in common cancers
Biomarkers currently have a role in the prediction or diagnosis of a number of common cancers (Table 2).
Breast Cancer
Breast cancer can be used to illustrate the contribution of molecular diagnostics to personalised treatment. Discovered in the 1970s, tamoxifen was the first targeted cancer therapy against the oestrogen signalling pathway. [8] Approximately three quarters of breast cancer tumours express hormone receptors for oestrogen and/or progesterone. Modulating either the hormone ligand or the receptor has been shown to be effective in treating hormone receptorposi tive breast cancer for over a century. Although quite effective for a subset of patients, this strategy has adverse partial oestrogenic eff ects in the uterus and vascular system, resulting in an increased risk of endometrial cancer and thromboembolism. [9,10] Alternative approaches to target the ligand production instead of the ER itself was hypothesised to be more effective with fewer side effects. Recent data suggest that the use of specific aromatase inhibitors (anastrozole, letrozole and exemestane), which block the formation of endogenous oestrogen, may be superior in both the adjuvant [24] and advanced disease settings. [25]
Lung Cancer
Lung cancer is the most common cause of cancer-related mortality affecting both genders in Australia. [26] Many investigators are using panels of serum biomarkers in an attempt to increase sensitivity of prediction. Numerous potential DNA biomarkers such as the overactivation of oncogenes, including K-ras, myc, EGFR, and Met, or the inactivation of tumour suppressor genes, including p53 and Rb, are being investigated. Gefitinib was found to be superior to carboplatin– paclitaxel in EGFR-mutant non-small cell lung cancer cases [20] and to improve progression-free survival, with acceptable toxicity, when compared with standard chemotherapy. [27]
Melanoma
Australia has the highest skin cancer incidence in the world. [28] Approximately two in three Australians will be diagnosed with skin cancer before the age of 70. [29] Currently, the diagnosis and prognosis of primary melanoma is based on histopathologic and clinical factors. In the genomic age, the number of modalities for identifying and subclassifying melanoma is rapidly increasing. These include immunohistochemistry of tissue sections and tissue microarrays and molecular analysis using RT-PCR, which can detect relevant multidrug resistance-associated protein (MRP) gene expression and characterisation of germ-line mutations. [30] It is now known that most malignant melanomas have a V600E BRAF mutation. [31] Treatment of metastatic melanoma with PLX4032 resulted in complete or partial tumour regression in the majority of patients. Responses were observed at all sites of disease, including the bone, liver, and small bowel. [32]
Leukaemia
Leukaemia has progressed from being seen merely as a disease of the blood to one that consists of 38 different subtypes. [33] Historically a fatal disease, chronic myeloid leukaemia (CML) has been redefined by the presence of the Philadelphia chromosome. [34] In 1998, imatinib was marketed as a tyrosine kinase inhibitor. This drug has proven to be so effective that patients with CML now have mortality rates comparable to those of the general population. [35]
Colon Cancer
Cetuximab was the first anti-EGFR monoclonal antibody approved in the US for the treatment of colorectal cancer, and the first agent with proven clinical efficacy in overcoming topoisomerase I resistance. [22] In 2004, bevacizumab was approved for use in the first-line treatment of metastatic colorectal cancer in combination with 5-fluorouracil-based chemotherapy. Extensive investigation since that time has sought to define bevacizumab’s role in different chemotherapy combinations and in early stage disease. [36]
Lymphoma
Another monoclonal antibody, rituximab, is an anti-human CD20 antibody. Rituximab alone has been used as the first-line therapy in patients with indolent lymphoma, with overall response rates of approximately 70% and complete response rates of over 30%. [37,38] Monoclonal antibodies directed against other B-cell-associated antigens and new anti-CD20 monoclonal antibodies and anti-CD80 monoclonal antibodies (such as galiximab) are being investigated in follicular lymphoma. [39]
Implication and considerations of personalised cancer treatment
Scientific considerations
Increasing information has revealed the incredible complexity of the cancer tumourigenesis puzzle; there are not only point mutations, such as nucleotide insertions, deletions and SNPs, but also genomic rearrangements and copy number changes. [40-42] These studies have documented a pervasive variability of these somatic mutations, [7,43] so that thousands of human genomes and cancer genomes need to be completely sequenced to have a com¬plete landscape of causal mutations. And what about epigenetic and non-genomic changes? While there is a lot of intense research being conducted on the sorts of molecular biology techniques discussed, none have been prospectively validated in clinical trials. In clinical practice, what use is a ‘gene signature’ if it provides no more discriminatory value than performance status or TNM-staging?
Much research has so far been focused on primary cancers; what about metastatic cancers, which account for considerable mortality? The inherent complexity of genomic alterations in late-stage cancers, coupled with interactions that occur between tumour and stromal cells, means that most often we are not measuring what we are treating. If we choose therapy based on the primary tumour, but we are treating the metastasis, we are likely giving the wrong therapy. Despite our increasing knowledge about metastatic colonisation, we still hold little understanding of how metastatic tumour cells behave as solitary disseminated entities. Until we identify optimal predictors for metastases and an understanding of the establishment of micrometastases and activation from latency, personalised therapy should be used sagaciously.
In addition, from a genomic discovery, it is difficult, costly and timeconsuming to deliver to patients a new targeted therapy with suitable pharmacokinetic properties, safety and demonstrable efficacy in randomised clinical trials. The first cancer-related gene mutation was discovered nearly thirty years ago – a point mutation in the HRAS gene that causes a glycine-to-valine mutation at codon twelve. [44,45] The subsequent identification of similar mutations in the KRAS family [46- 48] ushered in a new field of cancer research activity. Yet it is only now, three decades later, that KRAS mutation status is affecting cancer patient management as a ‘resistance marker’ of tumour responsiveness to anti-EGFR therapies. [21]
Ethical and Moral Considerations
The social and ethical implications of genetic research are significant, in fact 3% of the budget for the Human Genome Project is allocated for the same reason. These worries range from “Brave New Worldesque” fears about the beginnings of “genetic determinism” to invasions of “genetic privacy”. An understandable qualm regarding predictive genetic testing is discrimination. For example, if a person is discovered to be at genetically-predisposed to developing cancer, will employers be allowed to make such individuals redundant? Will insurance companies deny claims on the same basis? In Australia, the Law Reform Commission’s report details the protection of privacy, protection against unfair discrimination and maintaining ethical standards in genetics, of which the majority was accepted by the Commonwealth. [49,50] In addition, the Investment and Financial Services Association states that no applicant will be required to undergo a predictive genetic test for life insurance. [51] Undeniably, the potentially negative psychological impact of testing needs to be balanced against the benefits of detection of low, albeit significant, genetic risk. For example, population-based early detection testing for ovarian cancer is hindered by an inappropriately low positive predictive power of existing testing regimes.
As personalised medicine moves closer to becoming a reality, it raises important questions about health equality. Such discoveries are magnifying the disparity in the accessibility of cancer care for minority groups and the elderly, evidenced by their higher incidence rates and lower rates of cancer survival. This is particularly relevant in Australia, given the pre-existing pitfalls of access to medical care for Indigenous Australians. Even when calibrating for later presentations and remoteness, there have still been significant survival disparities between the Indigenous and non-Indigenous populations. [52] Therefore, a number of questions remain. Will personalised treatment serve only to exacerbate the health disparities between the developing and developed world? Even if effective personalised therapies are proven through clinical trials, how will disadvantaged populations access this care given their difficulties in accessing the services that are currently available?
Economic Considerations
The next question that arises is: Who will pay? At first glance, stratifying patients may seem unappealing to the pharmaceutical industry, as it may mean trading the “blockbuster” drug offered to the widest possible market for a diagnostic/therapeutic drug that is highly effective but only in a specific patient cohort. Instead of drugs developed for mass use (and mass profi t), drugs designed through pharmacogenomics for a niche genetic market will be exceedingly expensive. Who will cover this prohibitive cost – the patient, their private health insurer or the Government?
Training Considerations
The limiting factor in personalised medicine could be the treating doctor’s familiarity with utilising genetic information. This can be addressed by enhancing genetic ‘literacy’ amongst doctors. The role of genetics and genetic counselling is becoming increasingly recognised, and is now a subspecialty within the Royal Australian College of Physicians. If personalised treatment improves morbidity and mortality, the proportion of cancer survivors requiring follow-up and management will also rise, and delivery of this service will fall on oncologists and general practitioners, as well as other healthcare professionals. To customise medical decisions for a cancer patient meaningfully and responsibly on the basis of the complete profile of his or her tumour genome, a physician needs to know which specific data points are clinically relevant and actionable. For example, the discovery of BRAF mutations in melanoma [32] have shown us the key first step in making this a reality, namely the creation of a clear and accessible reference of somatic mutations in all cancer types.
Downstream of this is the education that medical universities provide to their graduates in the clinical aspects of genetics. In order to maximise the application of personalised medicine it is imperative for current medical students to understand how genetic factors for cancer and drug response are determined, how they are altered by genegene interactions, and how to evaluate the significance of test results in the context of an individual patient with a specific medical profile. Students should acquaint themselves with the principles of genetic variation and how genome-wide studies are conducted. Importantly, we need to understand that the same principles of simple Mendelian genetics cannot be applied to the genomics of complex diseases such as cancer.
Conclusion
The importance of cancer genomics is evident in every corner of cancer research. However, its presence in the clinic is still limited. It is undeniable that much important work remains to be done in the burgeoning area of personalised therapy; from making sense of data collected from the genome-wide association studies and understanding the genetic behaviour of metastatic cancers to regulatory and economic issues. This leaves us with the parting question, are humans just a sum of their genes?
Conflicts of interest
None declared.
Correspondence
M Wong: may.wong@student.unsw.edu.au