Abstract
Background:
Evidence of bullying and harassment of medical students and junior doctors has existed for over 30 years. However, there has been little attempt to explore the dimensions of this issue in Australia to date. Given the evidence which indicates that experiencing abusive behaviour has a detrimental effect on professional identity formation and on mental health, the Australian Medical Students’ Association (AMSA) undertook a national scoping study to better understand the experiences of Australian medical students.
Methods:
We conducted a mixed methods survey of the 16,959 students enrolled in a medical degree at an Australian university in 2015. An anonymous, voluntary online questionnaire was distributed through AMSA’s social media, email newsletter and website, and medical students’ societies.
Results:
We received 519 responses, including 194 (37%) detailing at least one incident of bullying or harassment. 335 (65%) survey respondents were women and 345 (67%) were in the clinical years of their training. 60% of all respondents reported experiencing or witnessing mistreatment during their medical education. The most common theme in the free text was belittlement of the student’s competence and capacity to be a good doctor. Some gave details about how universities failed to prevent or appropriately respond to students’ experiences of bullying and harassment.
Conclusion:
In line with international data, this study shows that many Australian medical students perceive mistreatment as an important problem that is not always managed well by faculties. Multi-pronged policy and practice responses are needed to instigate cultural change in Australian medical education.
Introduction
“How can we care for our patients, man, if nobody cares for us?”
— Chuck the Intern, The House of God, Samuel Shem [1].
Evidence of bullying of medical students and junior doctors has existed for over 30 years in the United States and the United Kingdom [2-7]. In Australia over the past two years, the topics of bullying, teaching by humiliation, and sexual harassment in Australian medical training have attracted attention both from the mainstream news media and within the profession. There is also some formal evidence about the extent of this problem nationally. A recent local study of “teaching by humiliation” found 74% of medical students reported experiencing this practice and 84% witnessed it [5].
Worldwide, similar studies have shown that any student can be affected, regardless of gender or race [8-10]. The most common form of mistreatment reported is covert, mostly in the form of belittling, exclusion or humiliation, rather than overt yelling or violence [4-6,11]. Sexual harassment is the most common form of documented incident [12-14]. The perpetrators of bullying are most commonly senior male clinicians [4,15]. Under-reporting is the norm, especially when the perpetrator of mistreatment is the student’s clinical supervisor, due to fears about the possible impact on career progression [4,10].
There is evidence that experiencing abusive behaviour causes harm both to the student and later, potentially, to their patients (and colleagues). Other research has demonstrated how a student’s developing identity affects their subsequent career progress, employability, and performance [17-19].
Mistreatment may be a contributor to the high levels of psychological distress found among medical students. Studies have shown that rates of such distress are three times higher among medical students than the general population (9.2% and 3.1% respectively), and that female medical students were more likely than male students to have considered suicide in the past twelve months, with 4.5% having attempted suicide. In particular, Indigenous students found bullying to be a substantial source of stress [16].
The exact nature of bullying and discrimination can be difficult to define. Through this research, we determined which incidents students found distressing, and what they considered to be bullying or discriminatory behaviour.
Prompted by an increase in reports of mistreatment from Australian medical students following media attention to the issue, the Australian Medical Students’ Association (AMSA), in association with the Sydney School of Public Health (SSPH), undertook scoping research to better understand the experiences of Australian medical students.
Rather than confirm the prevalence of abuse, demonstrated by previous research and by the Report of the Senate Inquiry into Medical Complaints Processes (2016) [20], we aimed to explore aspects of students’ experiences and their responses.
Methods
Study design and sample
As the only other previous survey of this issue in Australia was distributed to students from two medical schools only [5], our study aimed to reach a wide variety of students from all Australian medical schools and to confirm that previously published findings were generalisable nationally. For this reason, a survey was chosen as the medium for this research as it could be easily disseminated nationally online.
Medical students aged 18 and older who were enrolled in an Australian University between the 25th of August and the 5th of November 2015 were surveyed. The survey was an anonymous, voluntary online questionnaire using REDCap survey software (Vanderbilt University, Tennessee, USA) (see Supplementary Materials online).
The survey link and description were distributed through AMSA’s official Facebook page, Twitter account, website, and email newsletter (“Embolus”). Some medical schools’ student societies, as well as individual participants also shared the survey link.
The questionnaire contained four parts. Part one collected demographic information. In part two, respondents rated their perception of the extent of five categories of mistreatment — “general bullying”, “sexism”, “disability discrimination” (including mental illness), “racism”, and “homophobia” — in Australian medical education, by moving a pointer on a scale from 0 to 100. In part three, respondents rated the attributes of incidents they had witnessed or experienced and were then invited to use free text boxes to describe these incidents. They were also asked about their response to these incidents. In part four, students could describe what actions they felt AMSA could take in response.
The project received ethics approval from the Human Research Ethics Committee (HREC) of the University of Sydney [Protocol number 2015/642].
Data and statistical analysis
Basic demographic information about the respondents was reported, along with the proportions who reported experiencing or witnessing mistreatment. We tested whether experiencing or witnessing mistreatment was associated with gender, age, enrolment, sexuality, and training stage using Fisher’s exact test and Pearson’s chi-squared test. Boxplots were created based on the levels of agreement scales in part two. Differences in levels of agreement between subgroups of respondents were tested using two-sided exact Wilcoxon rank sum tests (gender, enrolment, and sexuality) and Kruskal-Wallis test (age), as the data were negatively skewed (Figure 2). These analyses were performed in R version 3.2.4 [21]. No adjustment has been made for multiple statistical comparisons.
Authors A-KS, EB and KI independently conducted an initial close coding of the open text responses with advice from CH. The taxonomies and categories developed in this process were then reviewed by the research team for comparison and reliability, and a primarily taxonomic thematic coding structure was agreed upon [22,23]. This was then applied to the free text data.
Results
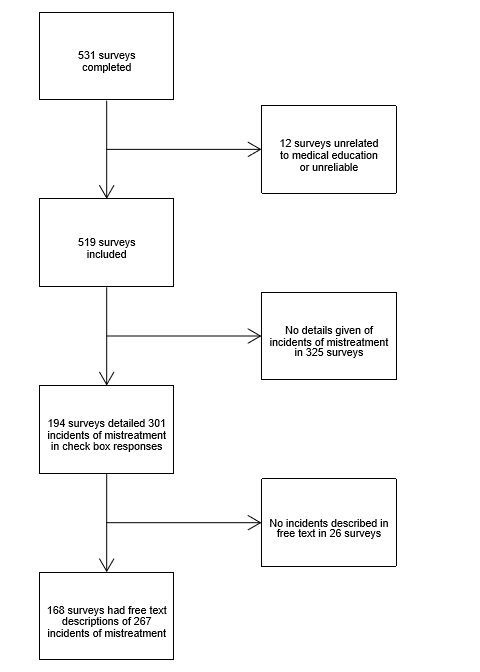
We received 531 completed surveys. Twelve surveys (2%) were excluded as they contained demonstrably unreliable answers or answers unrelated to medical education, leaving a sample of 519 surveys (Figure 1). The respondents were predominantly female (65%), young (median age of 24 years), local students (90%), and at the clinical stage of their training (67%) (Table 1). Each Australian medical school was represented.
It was reported by 60% of all respondents that they had witnessed or experienced adverse treatment (Table 1). Adverse treatment was more likely to be reported by: female than male students (64% vs 53%), older than younger students (79% for 35 years and older vs 55% for 20-24 years), non-heterosexual than heterosexual students (75% vs 58%), and clinical than pre-clinical students (70% vs 40%).
For the five categories of mistreatment (general bullying, sexism, disability discrimination including mental illness, racism, and homophobia), females reported greater problems in medical education than males (p≤0.004) (Figure 2). Non-heterosexuals tended to report greater problems than heterosexuals, particularly regarding homophobia (p<0.001). International students believed mistreatment was less of an issue in medical education than local students for all categories, except racism, though differences were small (p>0.05), and there were no consistent patterns with age (data not presented).

Information about 301 incidents involving mistreatment was given by 194 students (Figure 1). In 92% of incidents, the victim was a student (Table 2). The respondents nominated consultants as the primary instigator in 46% of the incidents. Belittlement, condescension or humiliation were present in 65% of the incidents. Most students (68%) reported they did not react (that is, take action in response) to the event. Two major reasons for not reacting were not knowing what to do, and fear of repercussions. Most students were bothered by the incident, with only 4% moving the slider scale from “a little” bothered to “not at all”. Over a third moved the slider to the lowest tenth of the scale, described as “very much”.

Reported p values are for tests of independence between experiencing/witnessing mistreatment and gender, age, enrolment, sexuality and training. Fisher’s exact test was used for gender and training, and Pearson’s chi-squared test for enrolment, sexuality and training.
*There is 1 missing value.
Of the 519 respondents, 168 submitted text descriptions of individual events (Figure 1). Of these, 41 described two events, 14 described three events, and ten described four events. In total, 267 events were described. Themes captured by coding the text responses included the type of event, the perpetrator, the situation and context, aspects that compounded the situation, and any potential outcomes of the event.
The most common theme was the denigration of the student’s competence and capacity to be a good doctor.
“The senior registrar in this instance verbally abused the student regularly, claiming that it was inconceivable that she would one day be a doctor and would cause great harm to potentially anyone she would treat.”
A commonly used framing motif was that the recipient was unworthy, should not have been allowed entry into medical school, or should make way for those who are actually fit to be doctors. The stories included examples of discrimination in all the social categories we investigated. One of the most common was the perceived incompetence or unworthiness of women.
“When we got it wrong, he would tell us we were stupid, we should drop out of medicine because we’d never make a good doctor, or there was no point trying, because we’d quit later to have babies like women should.”
“I was a new mother… and was told by another student I should be at home looking after my child instead of wasting a place at medical school that would have been better off given to someone else.”
A minority of the comments were on non-medical themes such as attractiveness, racial stereotypes, or perceived promiscuousness of the student.
“I would hear jibes about ‘Indians taking over the healthcare system of Australia’ and how ‘No one could understand their curry accent so they shouldn’t be able to work in this country.”
“All the women in our class [were] being scaled on ‘crazy versus hot.’ [The respondent was] followed into a women’s toilet and told to get down on my knees and ‘suck my dick’ while [a male medical student] grabbed his crotch.”
The more the abuse was related to medical practice or competence, the more respondents constructed it as acceptable or understandable.
“The taunts were often unrelated to medicine which made it even more unprofessional.”
Harm and suffering
Implicitly or explicitly, almost all of the 267 free text stories indicated that the recipient(s) of mistreatment were negatively affected as a result. Some accounts directly indicated that teaching by humiliation inhibited rather than enhanced medical learning, decreasing confidence and stopping the student from seeking out further educational opportunities from medical staff.
“Instead of attempting to teach the student in any way, she would harangue the student with increasingly difficult questions — lambasting her further with every question she answered incorrectly… this destroyed the confidence of the student in question quite quickly, to the point where she was afraid and unwilling to go to her clinical placement and learn for fear of the treatment she would receive the next day.”
“I understand that his motivation is to encourage us to be thorough, safe doctors. However, I was so scared at being yelled at for getting an answer wrong in his tutorials that I didn’t learn anything.”
Perpetrators
Students
Of the 38 responses indicating students as perpetrators, the same frame of medical incompetence and unworthiness was common.
“A fellow student kept on telling me that I was stupid and inept and kept saying things like if you don’t know this that (sic) you [don’t] belong in medicine … he threatened to hit me if I continue (sic) doing idiotic things.”
Faculty
We did not include the faculty as perpetrators in our questionnaire. Nevertheless, we received 22 responses citing medical school faculty (including both non-clinical staff and clinical staff in non-clinical roles) as reported perpetrators. These most often related to mishandling of reports of bullying, refusal, or inability to make reasonable allowances for mental illness or disability, and instances of discrimination against students.
“I was told that I was at risk of failing, had my depression called ‘your condition’ the whole time, making me think it was dirty or bad since it couldn’t even be addressed … They said to ask them any questions and the school of medicine would do everything it could to support me, but when I directly asked what they could offer they had nothing.”
Some respondents expressed disappointment and frustration at feeling unsupported by staff.
“The direct inaction by my university nearly led to my suicide … For me the only way I thought the Uni would notice my problem would be if I was to kill myself. Thankfully I pulled myself out of it and am still fighting week in week out to keep myself going.”
Often, students reported faculty promising support to the student, but providing no support or enacting no change. Other responses cited direct bullying or discriminatory action from the faculty towards the student.
“We get mistreated by the very people that are in control of our assessment/progression. How can you complain against the very person that controls your future? It’s just easier to endure it.”

Table 2. Details of 301 incidents of mistreatment reported by 194 medical students.
*The number of incidents with this question answered. **More than one response could be selected therefore the percentages do not sum to 100. *** “Other” includes (from most to least frequently reported) intrusive/unwanted questions, refusal to make reasonable allowance for the needs of others, threatening failure/low grade, receiving lower evaluations/grades, asking to perform personal/inappropriate tasks, spreading malicious rumours, being coerced into unprofessional behaviour, other, and actual/threatened physical punishment. **** “Other” includes (from most to least frequently reported) not there at the time, other, chalked it up to experience, told not to respond, it wasn’t that bad, didn’t have the time, my fault, didn’t care, not intentional, not important, and the data field not being filled in.
Discussion
Our study indicates that a significant proportion of medical students across the country experience or witness mistreatment, extending existing evidence of this issue, which had been previously confined to only two Australian medical schools. In line with other studies [4,11,24], our study shows that bullying and discrimination are commonly “medically themed”, in ways that belittle a student’s core identity and competency. This fits with sociologies of medicine that have shown that surviving humiliating treatment is often a ritual of socialisation into the profession [25]. Our study also extends our understanding of which students are affected and identifies a wider range of perpetrators than had earlier studies [5,14], including professional and support staff in their clinical schools and other students.
A limitation of our study was the sliding response scale for which the default setting was in the middle of the scale. If the respondent did not touch the slider, we could not be sure if they had elected to forego answering the question entirely (because they did not have an opinion or they did not want to answer) or if they were agreeing with the default mid-range answer.
While our low response rate and methods of recruitment mean that our results cannot be regarded as necessarily representative of the whole Australian medical student population, our data strengthen worldwide trends and provides confirmation that Australian medical students often experience serious mistreatment. It also reflects the findings of the Inquiry into Medical Complaints Processes, released in December 2016 [20,26].
Our study underscored that these behaviours can be damaging to students’ mental health. Our data also confirmed the widespread reluctance to disclose, report, or confront mistreatment as students fear direct educational and professional disadvantage as a result.
This research demonstrates that mistreatment is justified by the idea of upholding professional competence in medical students. It has also shown that, for some students, the mistreatment has a negative effect on their mental health and their willingness to perform. While there will be no single intervention solution for this problem, the authors suggest that clinical teaching staff may find an evidence-based short course on adult education and effective and constructive criticism, useful training for teaching medical students. This could include clear guidelines for both staff and students on the difference between effective teaching and bullying. Indeed, as teaching is often considered an integral part of clinical medicine, targeted preparation for this could commence in medical school. This should be paired with effective policies ensuring that staff who have been reported repeatedly for bullying behaviours are removed from teaching positions and receive appropriate training to improve their skills before resuming work.
We also saw that under-reporting is often due to fear of educational and professional disadvantage. We can address this by encouraging the production of university and hospital policies ensuring anonymity and protection for those who report, and providing alternatives such as switching the student to a different rotation.
Another finding was how some students felt that universities were failing to take action to support them. This was particularly linked to students with a disability or mental health conditions. The reports detail either a perceived choice by the university to not support the student or the admission that university staff did not have the ability or resources to support the student.
The authors suggest that universities enact stronger policies with safety nets available for struggling students (such as changing rotations, alternate exam arrangements, or taking time off) and ensure they have the necessary resources to do so. We also suggest the creation of policies that monitor how many students are struggling, detailing the issues, and taking steps to ensure the problem does not continue. The authors suggest that medical school accreditation processes should include a more rigorous examination of institutional performance on this issue.
These recommendations run alongside those handed down by the Inquiry into Medical Complaints Processes, which specifically identified the government, hospitals, colleges, and universities as parties with responsibility for addressing bullying and harassment in the medical profession [26].
Changes in policy and training educators on effective criticism would be strengthened by slowly incorporating cultural change through encouraging positive professionalism training. Such programs use creative techniques such as acting skills to build core professional values and behaviours. They can also reveal the impact of bullying on others without directly shaming perpetrators or exposing victims [27-29].
Further research is required to determine the effectiveness of these approaches to change. It is as yet unknown whether a pre-emptive educational approach or more capacity to remove perpetrators from teaching roles would be most effective in reducing mistreatment. Further qualitative research would better capture the dimensions and effects of mistreatment, which may be experienced differently by male and female students, on the basis of mental health status, or with respect to sexuality or ethnicity. Such research could assist in identifying institutional barriers to managing poor behaviour among teaching and non-clinical staff, and identify the best strategies by which the effects of mistreatment in medical education can be ameliorated.
Acknowledgements
We thank Rita Shackel for her assistance with the ethics approval process.
Conflict of interest
None declared.
Correspondence
A Szubert: anna.szubert64@gmail.com
References
[1] Shem S. The House of God. New York: Dell Publishing Company; 1978.
[2] Baldwin Jr D, Daugherty SR, Eckenfels EJ. Student perceptions of mistreatment and harassment during medical school: a survey of ten United States schools. West J Med. 1991;155(2):140.
[3] Neville AJ. In the age of professionalism, student harassment is alive and well. Med Educ. 2008;42(5):447-8. doi:10.1111/j.1365-2923.2008.03033.x
[4] Rees CE, Monrouxe LV. A morning since eight of just pure grill: a multischool qualitative study of student abuse. Acad Med. 2011;86(11):1374-82. doi:10.1097/ACM.0b013e3182303c4c
[5] Scott K, Caldwell P, Barnes E, Barrett J. Teaching by humiliation and mistreatment of medical students in clinical rotations: a pilot study. Med J Aust. 2015;203(4):185. doi:10.5694/mja15.00189
[6] Silver HK. Medical students and medical school. JAMA. 1982;247(3):309-10.
[7] Ulusoy H, Swigart V, Erdemir F. Think globally, act locally: understanding sexual harassment from a cross-cultural perspective. Med Educ. 2011;45(6):603-12. doi:10.1111/j.1365-2923.2010.03918.x
[8] Fnais N, Soobiah C, Chen MH, Lillie E, Perrier L, Tashkhandi M, et al. Harassment and discrimination in medical training: a systematic review and meta-analysis. Acad Med. 2014;89(5):817-27. doi:10.1097/ACM.0000000000000200
[9] Wear D, Aultman JM, Borges NJ. Retheorizing sexual harassment in medical education: women students’ perceptions at five U.S. medical schools. Teach Learn Med. 2007;19(1):20-9. doi:10.1080/10401330709336619
[10] Babaria P, Abedin S, Berg D, Nunez-Smith M. I’m too used to it: a longitudinal qualitative study of third year female medical students’ experiences of gendered encounters in medical education. Soc Sci Med. 2012;74(7):1013-20. doi:10.1016/j.socscimed.2011.11.043
[11] Sheehan KH, Sheehan DV, White K, Leibowitz A, Baldwin DC. A pilot study of medical student ‘abuse’: student perceptions of mistreatment and misconduct in medical school. JAMA. 1990;263(4):533-7.
[12] McDonald P. Workplace sexual harassment 30 years on: a review of the literature. Int J Manag Rev. 2012;14(1):1-17. doi:10.1111/j.1468-2370.2011.00300.x
[13] Nora LM, McLaughlin MA, Fosson SE, Stratton TD, Murphy-Spencer A, Fincher R-ME, et al. Gender discrimination and sexual harassment in medical education: perspectives gained by a 14‐school study. Acad Med. 2002;77(12, Part 1):1226-34.
[14] White GE. Sexual harassment during medical training: the perceptions of medical students at a university medical school in Australia. Med Educ. 2000;34(12):980-6. doi:10.1097/ACM.0b013e3181d27fd0
[15] Crebbin W, Campbell G, Hillis DA, Watters DA. Prevalence of bullying, discrimination and sexual harassment in surgery in Australasia. ANZ J Surg. 2015;85(12):905-9. doi:10.1111/ans.13363
[16] Wu F, Ireland M, Hafekost K, Lawrence D; National mental health survey of doctors and medical students [Internet]. Beyond Blue; 2013 [cited 2015 Aug 25]. Available from: https://www.beyondblue.org.au/docs/default-source/research-project-files/bl1132-report—nmhdmss-full-report_web
[17] Foster C. Factors influencing notions of professionalism: insights from established practitioner narratives [dissertation]. Sydney (NSW): University of Sydney; 2012.
[18] Frost H, Regehr G. I am a doctor: negotiating the discourses of standardization and diversity in professional identity construction. Acad Med. 2013;88(10):1570-7. doi:10.1097/ACM.0b013e3182a34b05
[19] Monrouxe LV. Identity, identification and medical education: why should we care? Med Educ. 2010;44(1):40-9. doi:10.1111/j.1365-2923.2009.03440.x
[20] Medical complaints process in Australia [Internet]. Canberra: Community Affairs References Committee; 2016 Nov [cited 2017 Jan 16]. Available from
[21] R: A language and environment for statistical computing [Internet]. R Foundation for Statistical Computing: 2014 [cited 2015 Aug 25]. Available from: http://www.R-project.org/
[22] Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758-72. doi:10.12691/ajnr-1-1-2
[23] Creswell, JW. Research design – qualitative, quantitative and mixed methods approaches. 4th ed. California: SAGE Publications; 2014.
[24] Gan R, Snell L. When the learning environment is suboptimal: exploring medical students’ perceptions of mistreatment. Acad Med. 2014;89(4):608-17. doi:10.1097/ACM.0000000000000172
[25] Timm A. It would not be tolerated in any other profession except medicine: survey reporting on undergraduates’ exposure to bullying and harassment in their first placement year. BMJ Open. 2014;4(7). doi:10.1136/bmjopen-2014-005140
[26] Buisson E. We know the way, but is there the will to stop bullying? [Internet]. MJA Insight; 2017 Jan 21 [cited 2017 Jun 10]. Available from: https://www.doctorportal.com.au/mjainsight/2017/1/we-know-the-way-but-is-there-the-will-to-stop-bullying/
[27] Scott KM, Berlec Š, Nash L, Hooker C, Dwyer P, Macneill P, et al. Grace under pressure: a drama-based approach to tackling mistreatment of medical students. Med Humanit. 2017. 43(1):68-70. doi:10.1136/medhum-2016-011031
[28] Heru AM. Using role playing to increase residents’ awareness of medical student mistreatment. Acad Med. 2003;78(1):35-8. doi:10.1097/00001888-200301000-00008
[29] Heru AM. Teaching psychosomatic medicine using problem-based learning and role-playing. Acad Psychiatry. 2011;35(4):245-8. doi:10.1176/appi.ap.35











