Introduction: Radiation Therapy (RT) is a common treatment modality for cancer management. Due to specific licensing and expertise requirements, RT tends to be centralised in larger urban centres resulting in restricted geographical access for many. Several studies conducted have examined the relationship between distance to treatment and utilisation of RT, however there remains a gap in literature with regards to Australian geography, particularly in rural areas where land is vast and treatment facilities are few. This review aimed to address the question: “Does increased geographical distance to a RT facility act as a barrier to seeking treatment?” Methods: The SCOPUS and Cumulative Index of Nursing and Allied Health Literature (CINAHL) databases were searched for articles pertaining to geography, access, and radiotherapy for all cancer diagnoses. Specific inclusion criteria were applied and the quality of the studies were assessed. Results: Twelve studies were eligible for inclusion in the review. Of these, nine studies identified a negative relationship between distance to RT facility and RT treatment, one study determined a positive relationship between geographical distance and RT treatment, and two studies noted public transportation as a barrier to RT treatment. Conclusion: This review suggests that there may be an inverse association between distance to treatment and utilisation of RT. However, studies were limited by retrospective design and prospective studies are required before firm conclusions can be drawn. In order to apply these findings to rural Australian settings, it would be ideal to examine data in local areas to determine if these populations are serviced adequately and where there are areas of underutilisation of RT.

Introduction
Radiation Therapy (RT) is a common treatment modality for a multitude of cancer diagnoses. RT may be used for radical or palliative intent; to provide disease control or improve quality of life. [1] The radiation dose is fractionated, delivered daily over weeks, and can in some cases take as many as nine weeks to achieve prescribed radiation doses. [2-4] It is a highly technical treatment that uses imaging options such as: Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and Positron Emission Tomography (PET) scanning to accurately delineate the tumour volume. Utilising the skills of radiation oncologists and radiation therapists, a precise dose of radiation is delivered to this targeted volume, destroying cancer cells whilst sparing normal tissue where possible.
Radiotherapy requires multidisciplinary input, for example from nursing, medical oncology, palliative care, dietetics and speech pathology. [5,6] For many patients it is the treatment of choice and yields excellent five year survival rates for localised solid tumours. [7] Due to the specific quality control measures, equipment and licensing requirements, substantial cost of treatment machines and the expertise required, the location of RT facilities tends to be centralised in larger urban centres, subsequently restricting access to those located in more regional and rural areas. [3,8,9]
Despite its therapeutic advantages, there are several factors that patients may consider prior to attending RT facilities, one of which is accessibility. For many patients the distance to a RT facility and the protracted course of treatment means that RT is not a feasible option. Challenges in accessing RT may lead to suboptimal treatment and subsequently poor outcomes for cancer patients. [1,3,7] Several studies have investigated the association between geographical distance to radiotherapy and radiotherapy utilisation, however they are limited by small sample sizes and differ in their conclusions. Accordingly, a systematic review was conducted to assess whether greater geographical distance to a RT facility was a barrier to RT treatment.
Methods
Search-strategy
A search strategy was devised according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement. [10] The SCOPUS (incorporating 100% of Medline titles) and Cumulative Index of Nursing and Allied Health Literature (CINAHL) databases were searched using the following search terms: (geograph* distance OR access) AND (radiation therapy OR radiotherapy), from January 1, 2000 to June 26, 2013 applied to abstracts.
Inclusion criteria
Studies were included if factors associated with access to or inequalities in receiving RT or cancer treatment were noted on all diagnoses of cancer. Studies were included if they were in the English language, pertinent to humans and linked to publically available full text articles.
Exclusion criteria
Studies were excluded if the primary objective did not include geographical distance or access barriers to RT facility or cancer treatment; if the study focused on treatments rather than barriers to treatment; or if the data was published prior to 2000.
Data extraction and quality assessment
Studies were independently abstracted for quality assessment by the primary author with corroboration from co-authors. Quality assessment was based on the study design, sample size, control for confounders, and control of bias. [11,12] The studies were rated as high (H), moderate (M) or low (L) quality based on study design, execution, and reporting. High quality suggested a prospective study design with a large sample size, considerable control of confounders, and little bias, whereas low quality reflected a small sample size, limited control of confounders, and significant bias.
Results
The search of the SCOPUS database yielded 57 results, of which 22 met the eligibility criteria, with 11 that were relevant to geographical distance and variations in access to RT and available in full text. Repeating the search in CINAHL provided 39 additional results of which no articles were deemed relevant to the primary aims of this systematic review. One additional study was identified from grey literature searching and was included in the review, resulting in a total of 12 studies (Figure 1).

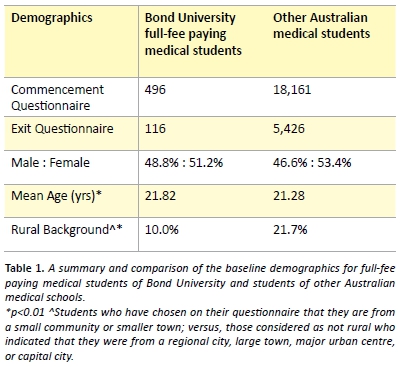
The quality of the included studies is shown in Table 1. As most of the studies were retrospective in study design where data examined was retrieved from cancer registries, they tended to be of moderate quality assessment. Overall, two studies were deemed to be high quality and ten studies were considered to be of moderate quality. None of the included studies were considered to be of poor quality.
The geographical location of each study is summarised in Table 2. Of the 12 studies, eight were conducted in the United States, one study was conducted in Canada, one study was conducted in the United Kingdom and two studies were conducted in Australia with a mixture of urban and rural settings. Several studies utilised geographic information system (GIS) software to map and measure the distance from the patient’s residence to the RT facility to give an indication of the accessibility of the RT clinics. Distances were calculated using straight line measurements rather than the actual route travelled by the patient via the software.
Of the 12 studies that met the inclusion criteria, nine identified a negative relationship whereby the greater the distance to the RT facility, the less likely the patient would be to undergo RT. [1,3,4,7-9,13-15] One prospective study with moderate control for confounders determined a positive relationship, whereby the greater the distance to the RT facility, the greater the likelihood of receiving RT. [16] There were two studies that did not address the distance to the RT clinic, but instead noted that lack of public transportation to RT facility was an access barrier, and that the presence of a radiation oncologist reduced mortality rates. [2,17] Although these two studies did not specifically address the primary objective, their results indicate that travel time to RT clinics is a major barrier to patients and that local resources such as radiation specialists can improve prognoses. Synthesis of the study data yielded a list of factors that were considered to influence access to RT (Box 1). The most influential factors contributing to radiotherapy access included: shorter distance to the RT facility, higher socio- economic status (SES), and increased education.

Discussion
The findings of this review suggest that geographical distance to RT facilities is a barrier to RT treatment. The majority of the studies included found that with increased distance to the RT facility, there was lower utilisation of RT as a treatment. One study conducted in Queensland, Australia reported conflicting findings, suggesting that with increasing distance to RT facilities there was higher utilisation of RT. This study focussed specifically on the prostate cancer population in Queensland, which is often an older population and therefore may have other factors that influence RT accessibility, such as retirement, income, and doctor preferences, whereas other studies often looked at cancer patient populations in younger cohorts. Older populations may not have to factor in time away from employment, and may have family they can reside with that live in regional centres. They may have previous exposure to hospitals and specialists, and therefore may have alternative factors that impact on preferences for location. [16] The findings of this study were potentially also limited by confounding bias as stated by the authors.
It is important to note that there was considerable variability in the geographical setting of the included studies. One study was conducted in a metropolitan city in the USA and the results may not be applicable to Australian settings. Interestingly, at least one study from each nation and the majority of research included in this review found that increased distance to RT facilities can act as a barrier to utilisation of RT, suggesting that this is a global phenomenon.
It would be useful to qualitatively investigate why patients select RT as their treatment option to ascertain insight into the barriers patients subjectively experience. With lower population density and lack of available RT facilities in rural areas such as Northern Queensland, there are great distances that must be traversed in order to receive life- saving treatment. Public transportation alone cannot be considered a barrier in instances where it is not available to patients, as is the case in remote areas. Therefore it is important to investigate area- specific geographical barriers, as rurality may pose other obstacles to overcome. It would also be interesting to explore whether variations exist in the acceptance of RT during the wet season when driving conditions could be challenging. This area of cancer care deserves much attention, especially in areas with vast land and few facilities. Identifying barriers to receiving RT is crucial to addressing the needs of the population.
Limitations of the studies synthesised in this review include the fact that many studies investigated distance to treatment rather than actual road travel times, which can vary significantly in many areas in Australia due to factors such as traffic, road works, the wet season and mountainous regions. There remains controversy in the optimal methodology used to assess accessibility to treatment. The GIS methods that were cited in this review were variable in their measurement of distance, often utilising straight line methods or mile radius buffer zones, which are not representative of the course travelled by the patient and do not give a clear indication of travel time. It is likely that increasing the accuracy of GIS distance measurements, by using round distance or alternatives as opposed to straight line measurements would exaggerate rather than minimise these differences.
This systematic review has a number of limitations. Firstly, two databases were utilised in the literature search and only open-access full text manuscripts were included, therefore restricting the amount of literature reviewed. Secondly, the methodological quality of the majority of included studies was moderate. The studies examined were either of retrospective or prospective study design. Most studies identified that the decision to proceed with RT is multifactorial, and many adjusted for a limited number of confounders. An ideal study would follow each patient with a diagnosis of cancer prospectively through a questionnaire or interview to ascertain which factors act as barriers or enablers to the decision for treatment. It would then revisit the patient post treatment to assess for any changes or additional challenges met. This would be a time-intensive process which would involve long follow up of patients, and may potentially be intrusive to patients during an emotional and difficult period in their life. Finally, the scope of the literature search was expanded to include all geographical locations rather than confining the search to rural areas in Australia alone due to the paucity of literature available. The results are therefore limited in their transferability to Australian settings.
Creating new technologies to deliver better dose profiles to tumour volumes is an integral part of radiation therapy, but however precise these treatments can be, their use is of limited value to populations who are not able to access RT. [18,19] Uniquely, radiotherapy will always need to be delivered in larger centres unlike other areas of oncology where initiatives such as tele-oncology are overcoming geographical access barriers. Therefore, further work in determining the role of innovative strategies to minimise the time patients spend away from home in rural areas and the burden associated with receiving treatment would be useful. [20,21]
Conclusion
Multiple factors are considered in the decision making process to have radiotherapy versus alternative treatments and these remain individual and context specific. Access to the RT facility is one important factor considered in this review. [22] The preference for modalities is important to investigate as studies have indicated a discrepancy between evidence based optimal and actual utilisation rates of RT. [1,23,24] The multitude of factors and social context that influences the patients’ choice for and satisfaction with treatment makes this a complex and significant area of research. [22,25] This review indicates that most likely rurality and increased distance from RT centres are important considerations, thus there is also the requirement for additional research into areas that may improve access for the rural cancer patient population, including travel subsidies, accommodation, and location of treatment facilities. However, there is a need for further studies, ideally prospective, and geography specific, before firm conclusions can be drawn.
Acknowledgements
The author would like to thank Associate Professor Sarah Larkins for her guidance and support. This research was conducted as part of a James Cook University School of Medicine Research Scholarship awarded in 2013.
Conflict of interest
None declared.
Correspondence
D K Sharma: divya.sharma@my.jcu.edu.au
References
[1] Soo J, French J, McGahan CE, Duncan G, Lengoc S. A retrospective study on accessibility of palliative radiation therapy in the management of prostate cancer in British Columbia. Journal of Radiotherapy in Practice. 2011;10(3):159-72.
[2] Aneja S, Yu JB. The impact of county-level radiation oncologist density on prostate cancer mortality in the United States. Prostate Cancer and Prostatic Diseases. 2012;15(4):391-6. [3] Schroen AT, Brenin DR, Kelly MD, Knaus WA, Slingluff Jr CL. Impact of patient distance to radiation therapy on mastectomy use in early-stage breast cancer patients. Journal of Clinical Oncology. 2005;23(28):7074-80.
[4] Voti L, Richardson LC, Reis IM, Fleming LE, MacKinnon J, Coebergh JWW. Treatment of local breast carcinoma in Florida: The role of the distance to radiation therapy facilities. Cancer. 2006;106(1):201-7.
[5] Bomford CK KI. Walter and Miller’s textbook of radiotherapy: radiation physics, therapy and oncology. 6 ed. USA: Churchill Livingstone Elsevier Ltd; 2003.
[6] Khan F. The physics of radiation therapy. 3 ed. USA: Lippincott Williams &Wilkins; 2003. [7] Cetnar JP, Hampton JM, Williamson AA, Downs T, Wang D, Owen JB, et al. Place of residence and primary treatment of prostate cancer: Examining trends in rural and nonrural areas in wisconsin. Urology. 2013;81(3):540-6.
[8] Athas WF, Adams-Cameron M, Hunt WC, Amir-Fazli A, Key CR. Travel distance to radiation therapy and receipt of radiotherapy following breast-conserving surgery. Journal of the National Cancer Institute. 2000;92(3):269-71.
[9] Underhill C, Bartel R, Goldstein D, Snodgrass H, Begbie S, Yates P, et al. Mapping oncology services in regional and rural Australia. Australian Journal of Rural Health. 2009;17(6):321-9.
[10] Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. British Medical Journal. 2009;339:b2535.
[11] Khan, Khalid S, Kunz R, Kleijnen J, Antes G. Five steps to conducting a systematic review. Journal of the Royal Society of Medicine. 2003;96(March 2003):118-21.
[12] Liamputtong P, editor. Research methods in health education Ch 18: Everything you wanted to know about systematic reviews. Sydney, NSW, Australia; 2010.
[13] Baldwin LM, Patel S, Andrilla CHA, Rosenblatt RA, Doescher MP. Receipt of recommended radiation therapy among rural and urban cancer patients. Cancer. 2012;118(20):5100-9.
[14] Boscoe FP, Johnson CJ, Henry KA, Goldberg DW, Shahabi K, Elkin EB et al. Geographic proximity to treatment for early stage breast cancer and likelihood of mastectomy. Breast. 2011;20(4):324-8.
[15] Williams MV, Drinkwater KJ. Geographical Variation in Radiotherapy Services Across the UK in 2007 and the Effect of Deprivation. Clinical Oncology. 2009;21(6):431-40.
[16] Baade P, Youlden DR, Gardiner RA, Ferguson M, Aitken JF, Yaxley J et al. Factors associated wth treatment received by men diagnosed with prostate cancer in Queensland, Australia. BJU International. 2012;110:712-9.
[17] Peipins LA, Graham S, Young R, Lewis B, Flanagan B. Racial disparities in travel time to radiotherapy facilities in the Atlanta metropolitan area. Social Science and Medicine. 2013;89:32-8.
[18] Delaney G, Jacob S, Featherstone C, Barton M. The role of radiotherapy in cancer treatment: Estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer. 2005;104(6):1129-37.
[19] Mackillop WJ, Groome PA, Zhang-Solomons J, Zhou Y, Feldman-Stewart D, Paszat L et Does a centralized radiotherapy system provide adequate access to care? Journal of Clinical Oncology. 1997;15(3):1261-71.
[20] Sabesan S, Larkins S, Evans R, Varma S, Andrews A, Beuttner P et al. Telemedicine for rural cancer care in North Queensland: Bringing cancer care home. Australian Journal of Rural Health. 2012;20(5):259-64.
[21] Sabesan S, Simcox K, Marr I. Medical oncology clinics through videoconferencing: An acceptable telehealth model for rural patients and health workers. Internal Medicine Journal. 2012;42(7):780-5.
[22] Gauthier DM, Swigart VA. The contextual nature of decision making near the end of life: Hospice patients’ perspectives. American Journal of Hospice and Palliative Medicine. 2003;20(2):121-8.
[23] Delaney G, Barton M, Jacob S. Estimation of an Optimal Radiotherapy Utilization Rate for Breast Carcinoma: A Review of the Evidence. Cancer. 2003;98(9):1977-86.
[24] Delaney G, Jacob S, Barton M. Estimating the optimal external-beam radiotherapy utilization rate for genitourinary malignancies. Cancer. 2005;103(3):462-73.
[25] Resnick MJ, Guzzo TJ, Cowan JE, Knight SJ, Carroll PR, Penson DF. Factors associated with satisfaction with prostate cancer care: Results from Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE). BJU International. 2013;111(2):213-20.