It is accepted that populations in the so-called developed world have gone through an ‘epidemiological transition’ where chronic disease has replaced infection as the primary cause of death. However, there is mounting evidence that infections play a key role in certain chronic diseases such as cancer. Cancers of infectious origin provide the perfect opportunity for harnessing the advances that have been made in the control of communicable diseases to attempt the control of noncommunicable diseases. Worldwide, one in every five malignancies can be attributed to infections: this figure is considered conservative and expected to rise. About two-thirds of these cancers occur in less developed countries. The majority of these malignancies are recognised to be caused by viruses via mechanisms of chronic inflammation, immunosuppression or the expression of oncogenic proteins. An understanding of virally mediated carcinogenesis may provide new targets for the development of specified viral therapy that not only impacts on viral infections but human cancer as well. From a public health perspective, viral carcinogenesis is important because it shows potential for preventative and therapeutic programmes to reduce the burden of cancer, particularly in less developed countries.
Introduction
The process of carcinogenesis involves multiple contributing factors. These include environmental, lifestyle, host factors, genetically inherited traits and infectious agents. Infectious agents are important from a public health aspect as they represent a significant and preventable cause of cancer. The infection-attributable cancer burden has been estimated at 1.9 million cases, or 17.8% of the total global cancer burden. [1] The percentage of infection-attributable cancer is higher in developing countries (26.3%) than in developed countries (7.7%), reflecting the higher prevalence of infectious diseases. Of these infection-associated cancers, viruses are the most common causative agents with 12.1% of cancers worldwide attributed to viral infections. [1]
 This article aims to outline current knowledge of the role of viruses in mediating cancer, explore the main mechanisms involved and propose exciting preventative and therapeutic approach for virus-associated cancers in the 21st century.
This article aims to outline current knowledge of the role of viruses in mediating cancer, explore the main mechanisms involved and propose exciting preventative and therapeutic approach for virus-associated cancers in the 21st century.
Mechanisms by which viruses mediate cancer
The International Agency for Research on Cancer (IARC) recognises seven viral agents that have been linked with cancer: Hepatitis B Virus (HBV) and Hepatitis C Virus (HCV), Human Papilloma Virus (HPV), Epstein-Barr Virus (EBV), Karposi-Sarcoma Herpes Virus (Human Herpes Virus 8), Human T-cell leukemia virus type I (HTLV-1) and Human Immunodeficiency Virus type 1 (HIV). [2] These seven viruses classified as ‘carcinogenic to humans’, and the recently discovered Merkel Cell Virus which has not yet been included by the IARC, are summarised in Table 1.
The induction of cancer development by viruses requires persistent infection of the host. It is hypothesised that long-term infection initiates cellular changes that predispose to cancer progression. [3]
In addition to persistent infection, the specific actions of these viruses are discussed below and can be broadly grouped into viruses that induce cancer by (i) chronic inflammation (eg. HCV), (ii) immunosuppression (eg. HIV) and by (iii) direct actions of viral oncogenic proteins (eg. EBV, HPV). [3]
(i) Cancer associated with chronic inflammation: Hepatitis B and C Viruses
Once a viral infection is initiated, recovery requires the activation of the innate and adaptive arms of the immune system. Acute inflammation is usually a short process that eliminates the pathogen. However, chronic inflammation may result if acute inflammation continues unresolved and fails to eradicate the pathogen. Chronic inflammation itself may promote carcinogenesis via the release of many factors including nitric oxide, cytokines and chemokines thus mediating DNA damage and effecting cell proliferation and neoangiogenesis. [3]
HBV and HCV infections are examples of chronic infections associated with ongoing inflammation. HBV and HCV are responsible for 54% and 31% of human hepatocellular carcinoma (HCC) cases worldwide. [4,5] These hepatotropic viruses can induce cirrhotic livers from which HCC can arise. This review will focus on HCV.
In those infected with HCV, 80% will develop chronic infection, and in 30 years 10-30% of these chronic HCV infections will develop cirrhosis. The subsequent rate of cirrhotic HCV liver disease developing HCC is 1-3% per year. [6] Since current WHO estimates suggest that 3% of the world’s population, or 150 million people, are HCV infected, this represents a significant virus-associated cancer burden.
HCV is a RNA virus of the hepacivirus family of the genus Flaviviridae. HCV does not integrate itself into the host genome and several viral proteins (core protein and the NS3, NS4B and NS5A) have been suggested as potential oncogenic candidates in-vitro. For example, the HCV NS5A protein has been shown to bind and sequester the cellular p53 protein to the perinuclear membrane, and it may be the be key to HCC development. [7] However, it is thought that HCC primarily occurs due to repeated rounds of hepatocyte destruction and regeneration from chronic inflammation, producing a procarcinogenic cirrhotic microenvironment, [3,8] rather than through the action of viral oncogenes. Cirrhosis appears to be the main risk factor for HCC, but exogenous factors could also play a role, such as chronic alcohol consumption, viral co-infection (such as HIV modulating immunosuppression), diabetes and obesity [4] highlighting the multifactorial triggers for the induction of cancer. [9]
HCV is also a well-established cause of essential mixed cryoglobulinemia, a lymphoproliferative disease that can evolve into B-cell non-Hodgkin lymphoma (NHL). [10] HCV has been suggested to be lymphotropic, but this is not well defined. [11] Again, since HCV has not been demonstrated to encode direct oncogenic proteins, the mechanisms of HCV-induced NHL are likely to be via chronic inflammation.
(ii) Cancer associated with immunosuppression and insertional mutagenesis: HIV
It is estimated that there are approximately 34.2 million individuals worldwide living with HIV infection, two-thirds of these being in sub-Saharan Africa. [12] People with HIV have a substantially higher risk of certain cancers compared with uninfected people of the same age. These cancers are termed AIDS-defining malignancies and include: Kaposi sarcoma, a mesenchymal tumour originating from lymphatic endothelial cells, cervical cancer and NHL. [13] Additionally, other types of cancer, such as Hodgkin’s disease (HD), anal cancer, lung cancer and testicular germ cell tumours appear to be more common among HIV-infected subjects compared to the general population and are termed AIDS-associated cancers. [14]
HIV is an RNA lentivirus of the Retroviridae family. The members of this family all integrate into the host chromosome and thus have the potential to cause direct insertional mutations or activation of cellular oncogenes. Other members of the Retroviridae family, such as Mouse mammary tumour virus (MMTV) have a well-defined link with tumours in mice, which are likely mediated by insertional activation of cellular genes in breast tissue through hormone responsive elements in the MMTV promoter. [15] Similarly, insertional mutagenesis and the induction of lymphoma has been identified in humans treated with gammaretrovirus [16] and lentivirus vectors used in gene therapy. [17] In contrast, there is little evidence for an HIV oncogenic protein, although studies have suggested that the transactivator protein of viral gene expression, Tat, which has oncogenic potential, is secreted by HIV. It has also been suggested that Tat can re-enter non-infected cells blocking apoptosis and accelerating tumour formation. [18]
The above described AIDS-associated cancers are linked with low CD4+ T-cell counts, and this may lead to co-infections with other oncogenic viruses such as HPV (cervical cancer) and Kaposi’s sarcoma-associated herpesvirus (Kaposi’s sarcoma), or the reactivation of existing infections with opportunistic oncogenic viruses such as EBV (Burkitt’s lymphoma). [18] However, the specific mechanisms by which depressed immunity may increase the risk for cancer are unclear, except for KS and most subtypes of NHL that are strictly associated with a low CD4 count. [19] Supporting the link between cancer and immunosuppression, the pattern of cancers in immunosuppressed organ transplant recipients is similar to people with HIV/AIDS. [20]
Thus, the evidence suggests that HIV can be associated with carcinogenesis through insertional mutagenesis. Moreover, HIV may indirectly cause cancers by inducing a chronic state of immunosuppression, reducing immunosurveillance for neoplastic cells, and increasing the risk of reactivation of latent oncogenic viruses as well as the risk of acquiring new oncogenic viral infections.
(iii) Cancer associated with Oncogenic viruses
Of the identified and accepted carcinogenic viruses, EBV, HHV-8, HTLV-1and HPV are tumour viruses that express viral oncogenic proteins to exert carcinogenesis. HBV also produces the HBx protein that disrupts signal transduction and deregulates cell growth: however, HBV-associated carcinogenesis is believed to be mainly mediated through chronic inflammation as described for HCV. [3] Oncogenic viruses can transform cells by carrying viral oncogenes into a cell or by activating cellular proto-oncogenes. [5] The virally derived oncogenes produce transforming growth factors that deregulate growth control and proliferation, leading to malignant transformation. Specific examples are discussed below, with the oncogenic viruses divided into DNA and RNA tumour viruses.
DNA Tumour Viruses
EBV best illustrates DNA tumour viruses. EBV is a double-stranded DNA virus of the herpesviridae family, and causes infectious mononucleosis. Like all herpesviruses, EBV causes a life-long latent infection, and EBV is the primary cause of B-cell transformation in Burkitt’s lymphoma. [14] This was the first human tumour associated with an infectious agent. Since then, EBV has been implicated in a number of other cancers (see Table 1).
In the case of EBV-lymphoma, expression of the viral oncogene, latent membrane protein-1 (LMP1), transforms cells into lymphoblasts by the disruption of cellular signal transduction. [3] In contrast, in most NPCs, the viral BamHI-A reading frame-1 (BARF1) gene is expressed. BARF1 has been identified as an important oncogene in NPC pathology. [21] Thus, EBV has a number of different oncogene expression profiles associated with different cancers. EBV is extremely widespread in prevalence affecting more than 90% of the world’s population, [22] yet only a small fraction of the infected populations have a cancer attributable to EBV. Therefore, beside viral factors, host responses also play a role in the neoplastic transformation of EBV-infected cells.
HHV-8 is a DNA virus of the herpesviridae family, and HHV-8 infection is strongly associated with Kaposi’s sarcoma. The mechanism, however, of HHV-8-induced carcinogenesis is very different to that of the related virus, EBV. HHV-8 infects endothelial cells and encodes a viral G protein-coupled receptor (vGPCR). This vGPCR has dysregulated signalling function and acts as an oncogene, inducing angioproliferative tumours. [23]
HPV is a DNA virus of the papillomavirus family, and there are 30-40 types. Approximately fifteen types of HPV are oncogenic viruses, causing 5.2% of total human cancers. [24] These cancers include those of the ano-genital mucosae (cervix, vagina, vulva, anus and penis), and the mouth and the pharynx. [24,25] The predominant transmission of these HPV infections is sexual. [26] While HPV is an accepted aetiological factor for oral and pharyngeal cancers, the major risk factors are tobacco and alcohol, with the effects of these exposures being multiplicative. [25] Oncogenic HPV can be detected by PCR in virtually all cases of cervical cancer, with specific genotypes HPV16 and 18 identified as the primary causes of cervical cancer. These viral genotypes have also been associated with 86-95% of HPV-associated non-cervical cancers. [26,27] These viruses infect the basal layer of the stratified epithelium and express two important viral oncoproteins, E6 and E7. [23] These proteins destabilise the cellular tumour suppressor genes, p53 and the retinoblastoma protein (RB). [28] This dysregulation of cellular growth directly leads to cell transformation and cancer.
RNA Tumour Viruses
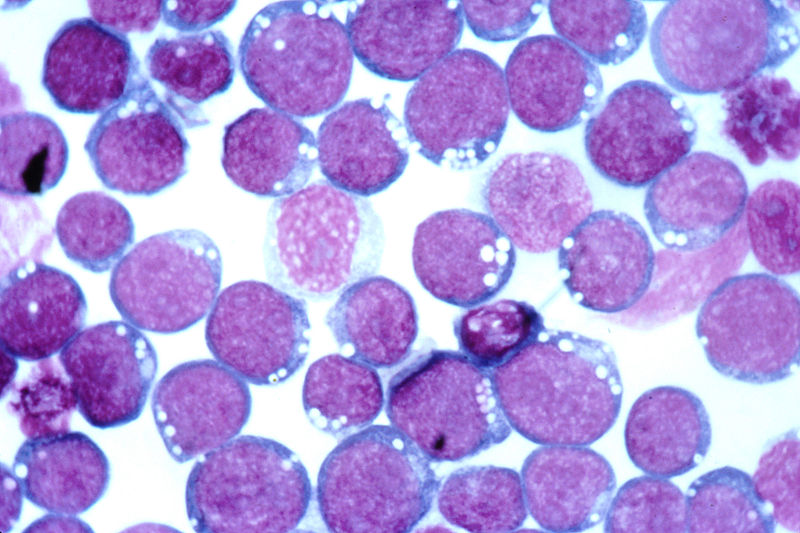
HTLV-I is a retrovirus related to HIV, which is associated with adult T-cell leukaemia. Only 1% of HTLV-I infected individuals will develop leukaemia, and only after a long latency period of 20-30 years. [29] HTLV-I infection rates are elevated in certain Indigenous populations of Central and Northern Australia, as well as the southern islands of Japan, the Caribbean basin and South Africa. [14] Unlike HIV, HTLV-I infections are not associated with immunosuppression, but HTLV-I encodes an oncogenic protein; the viral Tax protein. [30,31] Tax is a transcription factor and is known to bind to a number of cellular genes involved in cell cycle progression and growth regulation, such as NFkB and p53. [32] Via promotion of transcription and cell cycle progression, Tax is proposed to set up a self-stimulating loop that causes continuous proliferation of infected T-cells, and ultimately leukaemia.
The growing cancer burden attributable to viruses
While there are only seven viruses clearly recognised as carcinogenic to humans, this is conservative, with the discovery of new associations between infections, particularly viruses, and cancer anticipated.
MCV is a recently discovered DNA virus that is found to be associated with approximately 80% of Merkel Cell Carcinomas, an aggressive form of skin cancer. [33] MCV is a relatively common virus, yet only leads to cancer in rare circumstances. It is thought that this is because for MCV to become carcinogenic, two rare mutagenic steps must occur: viral integration and T antigen mutation. Integration of MCV is not a regulated event, unlike for HIV and HTLV-I, and occurs rarely. The integration, probably of only parts of the MCV genome into cells, renders the virus replication-incompetent, but allows parts of the virus, such as the T-antigens, to be maintained in these cells. [34] MCV T antigens can be oncogenic, and target cellular tumour suppressors and cell cycle regulatory proteins. Thus, the whole replicative virus may not be present, but the residual oncogenic T-antigen is, and can promote transformation of the cell leading to cancer.
Cancerous cells themselves are generally not transmissible. In humans, during the two known physiological routes for tumour cell transmission (pregnancy and organ transplantation), the immune system is altered. Transplacental transmission of lymphoma, acute leukaemia, melanoma and carcinoma have been observed, as well as acute leukaemia cells transmitted to the foetuses in multiple case pregnancies with the subsequent disease development in the newborn. [35] Similarly, in organ transplantation, donor derived tumour cells have been observed, with the immunosuppressive therapy following transplantation potentially facilitating the engraftment and growth of donor derived tumour cells. [35] Fortunately, these transmissible tumours are rare, with the development of donor-derived tumours in solid organ transplant recipients at 0.04%. [15] Additionally there have been rare case reports of human contagious cancers documented via needle stick (colonic adenocarcinoma), [36] and a surgeon contracting a malignant fibrous histiocytoma from a patient following an intraoperative cut to his left palm. [37]
Cancer prevention and public health strategies
In theory, the cancers resulting from viral infections represent an exciting potential for public health intervention strategies and therapeutics to prevent these cancers. In particular, the high number of cancers attributable to viral infections in developing countries presents a real need and opportunity for public health programs to reduce both infectious disease and cancer burden. [38]
The mode of transmission of the seven IARC-recognised carcinogenic viruses is provided in Table 2. The implementation of public health education, awareness, treatment and prevention programs to reduce the horizontal spread of these viruses and manage these viral infections in patients is a public health priority, but has the additional benefit of reduction in the associated cancer risks.
Public health programs should be prioritised to target vertical transmission of viral infections such as HBV and HIV. The WHO outlined targets and recommendations in 2010 with the prevention of mother to child transmission (PMTCT) strategy, targeting anti-retroviral therapy (ART) in pregnant women and providing guidelines for HIV in relation to infant breastfeeding. [39] Similar guidelines may be applicable to our Indigenous population afflicted by HTLV-I, which has a well described increased mother to child transmission rate associated with breastfeeding. [40] However, breastfeeding recommendations in resource poor settings need careful consideration. [41]
More outstanding, are the successful programs for screening and management of viral infections associated with cancer. For example, the National Cervical Screening Program (NCSP) in Australia has had a huge benefit in reducing the mortality rates from cervical cancer from 3.9/100,000 in 1991 to 1.9/100,000 in 2007, [42], demonstrating that cancer prevention via monitoring oncogenic viral infections is a real possibility. [43] Additionally, such programs as the NSW Cancer Council ‘B positive’ program, implemented in 2008 aims to increase HBV awareness and the treatment and management of chronic HBV infection to reduce the risk of HCC. [44]
Vaccination and treatments to prevent cancer-associated viral infections
Historically, the world has experienced, with polio and smallpox, elimination or virtual elimination of viral diseases through vaccination. There are now vaccines available for both HBV and HPV, two major infectious causes of HCC and cervical cancer, respectively. The HBV surface antigen is the basis for the vaccine against the HBV, which was first available in the 1980s, and is the first vaccine for prevention of a human cancer. [45] Vaccination programmes of children with the HBV vaccine have already proved successful in protecting against chronic carriage and HCC, [46,47] and HBV vaccination has now been introduced into the Australian childhood immunisation schedule. Long-term and full coverage of newborns against HBV has the potential of reducing HCC by approximately 85%. [14]
The two currently marketed vaccines for HPV utilise the L1 coat protein in the form of virus-like particles to prevent persistent infection with HPV16 and HPV18. [48-50] These viral subtypes are estimated to cause 71.8% of all HPV-related cancers, cervical and non-cervical. [25] These vaccines need to be administered prior to exposure to HPV16 and 18, which makes delivery in a public health setting more difficult than an infant setting. In Australia in 2007, the National HPV vaccination Program was made available to teenage women, and is now part of the school age vaccination program. From 2013 will also be made available to 12-13 year old males. [51] However, the current cost is not practical for all groups, especially those in developing countries, [14] and although the HPV vaccination program in developing countries is supported by the WHO, the applicability and benefits of HPV vaccination have been queried and recently suspended in India. [52] The efficacy of these HPV vaccines in preventing infections at sites other then the cervix, vagina and vulva should be assessed. [27] Specifically, research is required on the administration to high-risk groups (e.g. men who have sex with men and HIV positive people) for anal cancer. [24]
Unfortunately, the described RNA viruses associated with cancer, HIV and HCV, are highly genetically variable and therefore prove to be difficult candidates for prophylactic vaccines. For these viruses, anti-viral therapy appears to be more successful. For example, the risk of infection-associated cancers in HIV positive individuals is related to ongoing HIV replication. The use of suppressive highly active antiretroviral therapy (HAART) has dramatically reduced the risk for opportunistic infections and improved overall life expectancy in patients with HIV-infection and AIDS. [53] A significant decrease in the incidence of KS has been observed in patients treated with HAART. [19] Moreover, HAART and preserved CD4 count preferentially reduces the risk of malignancies associated with oncogenic infections. [54] Similarly, patients with HCV who were prescribed the anti-viral agent, interferon, showed regression of their splenic lymphoma. [55]
Recently approved HCV NS3-4A protease inhibitors are proving effective in clearing and curing HCV infection. In the future, this may significantly impact on HCV infection rates and subsequent incidence of HCC.
Exciting Therapeutic Targets
Our understanding of mechanisms of viral initiation of carcinogenesis has provided the opportunity to design innovative, targeted cancer therapies based on the pathways disrupted by the transforming viral genes.
For example, recent studies reveal that the cellular survivin oncoprotein is activated by MCV large T antigen protein via targeting the cellular Rb (p53) protein, and that survivin inhibitors can delay MCV-induced tumour progression in animal models. [56] Clinical trials are now in progress to determine whether these survivin inhibitors have any therapeutic benefits. Additionally, MCV is a target for cell-mediated immune responses, and so important research efforts are being focused on immunologic therapies that may benefit MCC patients. [56] These findings provide a proof of principle for specifically treating virus-associated cancers by targeting the mechanisms by which they induce oncogenesis. In the case of MCV, a promising rational drug target has been uncovered within only four years of the initial discovery of MCV as a causative cancer agent. Similarly, other new treatments for cancer might be rapidly developed should we identify new viral associations with malignancies.
Conclusion
Viruses are an important aetiological cause of human cancers, especially in the developing world where they lead to a significant burden of disease. Although viruses make an important contribution to human cancer development, it is often difficult to prove the association of viral infections with cancer, due to latency in tumour development and the multifaceted interaction with the host. It is reasonable to think that the calculations of cancers attributable to viruses are underestimates and that cancers other than the ones described may also be associated with viral infections. The viruses in this review exemplify the best-established human tumour viruses, but there are many other potential candidates. Undoubtedly, as our knowledge of carcinogenesis and viruses expand, further cancer-associated viruses will be discovered. From a public health point of view, infectious diseases are often preventable or treatable; therefore, cancers associated with infections are, or may become, preventable. Prevention may be in the form of vaccination, novel therapies to target the immune system or oncogenic proteins, or education and public health interventions.
Conflict of interest
None declared.
Correspondence
V Boon: boon0035@flinders.edu.au
References
[1] de Martel C, Ferlay J, Franceschi S, Vignat J, Bray F, Forman D, et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. 2012 Jun;13(6):607-15. PubMed PMID: 22575588. Epub 2012/05/12. eng.
[2] Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, et al. A review of human carcinogens–Part B: biological agents. Lancet Oncol. 2009 Apr;10(4):321-2. PubMed PMID: 19350698. Epub 2009/04/08. eng.
[3] Carrillo-Infante C, Abbadessa G, Bagella L, Giordano A. Viral infections as a cause of cancer (review). Int J Oncol. 2007 Jun;30(6):1521-8. PubMed PMID: 17487374. Epub 2007/05/10. eng.
[4] El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012 May;142(6):1264-73 e1. PubMed PMID: 22537432. Pubmed Central PMCID: 3338949. Epub 2012/04/28. eng.
[5] Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006 Jun 15;118(12):3030-44. PubMed PMID: 16404738. Epub 2006/01/13. eng.
[6] Rosen HR. Clinical practice. Chronic hepatitis C infection. N Engl J Med. 2011 Jun 23;364(25):2429-38. PubMed PMID: 21696309. Epub 2011/06/24. eng.
[7] Farazi PA, DePinho RA. Hepatocellular carcinoma pathogenesis: from genes to environment. Nat Rev Cancer. 2006 Sep;6(9):674-87. PubMed PMID: 16929323. Epub 2006/08/25. eng.
[8] Farazi PA, Glickman J, Horner J, Depinho RA. Cooperative interactions of p53 mutation, telomere dysfunction, and chronic liver damage in hepatocellular carcinoma progression. Cancer Res. 2006 May 1;66(9):4766-73. PubMed PMID: 16651430. Epub 2006/05/03. eng.
[9] Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology. 2004 Nov;127(5 Suppl 1):S35-50. PubMed PMID: 15508101. Epub 2004/10/28. eng.
[10] de Martel C, Franceschi S. Infections and cancer: established associations and new hypotheses. Crit Rev Oncol Hematol. 2009 Jun;70(3):183-94. PubMed PMID: 18805702. Epub 2008/09/23. eng.
[11] Zignego AL, Ferri C, Monti M, LaCivita L, Giannini C, Careccia G, et al. Hepatitis C virus as a lymphotropic agent: evidence and pathogenetic implications. Clin Exp Rheumatol. 1995 Nov-Dec;13 Suppl 13:S33-7. PubMed PMID: 8730474. Epub 1995/11/01. eng.
[12] Organisation WH. HIV/AIDS Fact Sheet No 360. Geneva WHO Media centre; 2011.
[13] Control CfD. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. Morb Mortal Wkly Rep. 1992;41:1-19.
[14] Harford JB. Viral infections and human cancers: the legacy of Denis Burkitt. Br J Haematol. 2012 Mar;156(6):709-18. PubMed PMID: 22233526. Epub 2012/01/12. eng.
[15] Braoudaki M, Tzortzatou-Stathopoulou F. Tumorigenesis related to retroviral infections. J Infect Dev Ctries. 2011 Nov;5(11):751-8. PubMed PMID: 22112727. Epub 2011/11/25. eng.
[16] Hacein-Bey-Abina S, Garrigue A, Wang GP, Soulier J, Lim A, Morillon E, et al. Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. J Clin Invest. 2008 Sep;118(9):3132-42. PubMed PMID: 18688285. Pubmed Central PMCID: 2496963. Epub 2008/08/09. eng.
[17] Cesana D, Sgualdino J, Rudilosso L, Merella S, Naldini L, Montini E. Whole transcriptome characterization of aberrant splicing events induced by lentiviral vector integrations. J Clin Invest. 2012 May 1;122(5):1667-76. PubMed PMID: 22523064. Pubmed Central PMCID: 3336994. Epub 2012/04/24. eng.
[18] Huynh D, Vincan E, Mantamadiotis T, Purcell D, Chan CK, Ramsay R. Oncogenic properties of HIV-Tat in colorectal cancer cells. Curr HIV Res. 2007 Jul;5(4):403-9. PubMed PMID: 17627503. Epub 2007/07/14. eng.
[19] Barbaro G, Barbarini G. HIV infection and cancer in the era of highly active antiretroviral therapy (Review). Oncol Rep. 2007 May;17(5):1121-6. PubMed PMID: 17390054. Epub 2007/03/29. eng.
[20] Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet. 2007 Jul 7;370(9581):59-67. PubMed PMID: 17617273. Epub 2007/07/10. eng.
[21] Decaussin G, Sbih-Lammali F, de Turenne-Tessier M, Bouguermouh A, Ooka T. Expression of BARF1 gene encoded by Epstein-Barr virus in nasopharyngeal carcinoma biopsies. Cancer Res. 2000 Oct 1;60(19):5584-8. PubMed PMID: 11034107. Epub 2000/10/18. eng.
[22] Liebowitz D. Nasopharyngeal carcinoma: the Epstein-Barr virus association. Semin Oncol. 1994 Jun;21(3):376-81. PubMed PMID: 8209269. Epub 1994/06/01. eng.
[23] Zheng ZM. Viral oncogenes, noncoding RNAs, and RNA splicing in human tumor viruses. Int J Biol Sci. 2010;6(7):730-55. PubMed PMID: 21152115. Pubmed Central PMCID: 2999850. Epub 2010/12/15. eng.
[24] Stanley MA, Winder DM, Sterling JC, Goon PK. HPV infection, anal intra-epithelial neoplasia (AIN) and anal cancer: current issues. BMC cancer. 2012;12:398. PubMed PMID: 22958276. Pubmed Central PMCID: 3488563.
[25] Parkin DM, Bray F. Chapter 2: The burden of HPV-related cancers. Vaccine. 2006 Aug 31;24 Suppl 3:S3/11-25. PubMed PMID: 16949997.
[26] Gillison ML, Castellsague X, Chaturvedi A, Goodman MT, Snijders P, Tommasino M, et al. Comparative epidemiology of HPV infection and associated cancers of the head and neck and cervix. Int J Cancer. 2013 Apr 9. PubMed PMID: 23568556.
[27] Gillison ML, Chaturvedi AK, Lowy DR. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer. 2008 Nov 15;113(10 Suppl):3036-46. PubMed PMID: 18980286.
[28] Baak JP, Kruse AJ, Garland SM, Skaland I, Janssen EA, Tabrizi S, et al. Combined p53 and retinoblastoma protein detection identifies persistent and regressive cervical high-grade squamous intraepithelial lesions. Am J Surg Pathol. 2005 Aug;29(8):1062-6. PubMed PMID: 16006801. Epub 2005/07/12. eng.
[29] Popovic M, Reitz MS, Jr., Sarngadharan MG, Robert-Guroff M, Kalyanaraman VS, Nakao Y, et al. The virus of Japanese adult T-cell leukaemia is a member of the human T-cell leukaemia virus group. Nature. 1982 Nov 4;300(5887):63-6. PubMed PMID: 6982418. Epub 1982/11/04. eng.
[30] Ding W, Albrecht B, Kelley RE, Muthusamy N, Kim SJ, Altschuld RA, et al. Human T-cell lymphotropic virus type 1 p12(I) expression increases cytoplasmic calcium to enhance the activation of nuclear factor of activated T cells. J Virol. 2002 Oct;76(20):10374-82. PubMed PMID: 12239314. Pubmed Central PMCID: 136546. Epub 2002/09/20. eng.
[31] Grassmann R, Aboud M, Jeang KT. Molecular mechanisms of cellular transformation by HTLV-1 Tax. Oncogene. 2005 Sep 5;24(39):5976-85. PubMed PMID: 16155604. Epub 2005/09/13. eng.
[32] Cheng H, Ren T, Sun SC. New insight into the oncogenic mechanism of the retroviral oncoprotein Tax. Protein Cell. 2012 Aug;3(8):581-9. PubMed PMID: 22865346. Pubmed Central PMCID: 3553852. Epub 2012/08/07. eng.
[33] Feng H, Shuda M, Chang Y, Moore PS. Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science. 2008 Feb 22;319(5866):1096-100. PubMed PMID: 18202256. Pubmed Central PMCID: 2740911. Epub 2008/01/19. eng.
[34] Shuda M, Feng H, Kwun HJ, Rosen ST, Gjoerup O, Moore PS, et al. T antigen mutations are a human tumor-specific signature for Merkel cell polyomavirus. Proc Natl Acad Sci U S A. 2008 Oct 21;105(42):16272-7. PubMed PMID: 18812503. Pubmed Central PMCID: 2551627. Epub 2008/09/25. eng.
[35] Welsh JS. Contagious cancer. Oncologist. 2011;16(1):1-4. PubMed PMID: 21212437. Pubmed Central PMCID: 3228048. Epub 2011/01/08. eng.
[36] Gugel EA, Sanders ME. Needle-stick transmission of human colonic adenocarcinoma. N Engl J Med. 1986 Dec 4;315(23):1487. PubMed PMID: 3785302. Epub 1986/12/04. eng.
[37] Gartner HV, Seidl C, Luckenbach C, Schumm G, Seifried E, Ritter H, et al. Genetic analysis of a sarcoma accidentally transplanted from a patient to a surgeon. N Engl J Med. 1996 Nov 14;335(20):1494-6. PubMed PMID: 8890100. Epub 1996/11/14. eng.
[38] Danaei G. Global burden of infection-related cancer revisited. Lancet Oncol. 2012 Jun;13(6):564-5. PubMed PMID: 22575586. Epub 2012/05/12. eng.
[39] Organisation WH. Mother-to-child transmission of HIV 2013. Available from: http://www.who.int/hiv/topics/mtct/en/.
[40] Moriuchi H, Masuzaki H, Doi H, Katamine S. Mother-to-child transmission of human T-cell lymphotropic virus type 1. Pediatr Infect Dis J. 2013 Feb;32(2):175-7. PubMed PMID: 23328821. Epub 2013/01/19. eng.
[41] van Tienen C, Jakobsen M, Schim van der Loeff M. Stopping breastfeeding to prevent vertical transmission of HTLV-1 in resource-poor settings: beneficial or harmful? Arch Gynecol Obstet. 2012 Jul;286(1):255-6. PubMed PMID: 22228317. Pubmed Central PMCID: 3374111. Epub 2012/01/10. eng.
[42] Welfare AIoHa. National Cervical Screening Program Key Statistics 2012. Available from: http://www.cancerscreening.gov.au/internet/screening/publishing.nsf/Content/facts.
[43] Frazer IH. Cervical cancer vaccine development. Sex Health. 2010 Sep;7(3):230-4. PubMed PMID: 20719210. Epub 2010/08/20. eng.
[44] NSW CC. About the B Positive Program Woolloomooloo NSW: Cancer Council NSW; 2013 [cited 2012 September 2012]. Available from: http://www.cancercouncil.com.au/52127/reduce-risks/cancer-screening-reduce-risks/b-positive-hepatitis-b-program/about-the-b-positive-program/.
[45] Blumberg BS. The discovery of the hepatitis B virus and the invention of the vaccine: a scientific memoir. J Gastroenterol Hepatol. 2002 Dec;17 Suppl:S502-3. PubMed PMID: 12534787. Epub 2003/01/22. eng.
[46] Whittle H, Jaffar S, Wansbrough M, Mendy M, Dumpis U, Collinson A, et al. Observational study of vaccine efficacy 14 years after trial of hepatitis B vaccination in Gambian children. BMJ. 2002 Sep 14;325(7364):569. PubMed PMID: 12228132. Pubmed Central PMCID: 124550. Epub 2002/09/14. eng.
[47] Ni YH, Huang LM, Chang MH, Yen CJ, Lu CY, You SL, et al. Two decades of universal hepatitis B vaccination in taiwan: impact and implication for future strategies. Gastroenterology. 2007 Apr;132(4):1287-93. PubMed PMID: 17433322. Epub 2007/04/17. eng.
[48] Harper DM. Why am I scared of HPV? CA Cancer J Clin. 2004 Sep-Oct;54(5):245-7. PubMed PMID: 15371282. Epub 2004/09/17. eng.
[49] Villa LL. Prophylactic HPV vaccines: reducing the burden of HPV-related diseases. Vaccine. 2006 Mar 30;24 Suppl 1:S23-8. PubMed PMID: 16194583. Epub 2005/10/01. eng.
[50] Lu B, Kumar A, Castellsague X, Giuliano AR. Efficacy and safety of prophylactic vaccines against cervical HPV infection and diseases among women: a systematic review & meta-analysis. BMC Infect Dis. 2011;11:13. PubMed PMID: 21226933. Pubmed Central PMCID: 3034689. Epub 2011/01/14. eng.
[51] Ageing AGDoHa. HPV School Vaccination Program Canberra2013 [cited 2012 September 2012]. Available from: http://hpv.health.gov.au/.
[52] Mattheij I, Pollock AM, Brhlikova P. Do cervical cancer data justify HPV vaccination in India? Epidemiological data sources and comprehensiveness. J R Soc Med. 2012 Jun;105(6):250-62. PubMed PMID: 22722970. Epub 2012/06/23. eng.
[53] Mocroft A, Devereux H, Kinloch-de-Loes S, Wilson D, Madge S, Youle M, et al. Immunological, virological and clinical response to highly active antiretroviral therapy treatment regimens in a complete clinic population. Royal Free Centre for HIV Medicine. AIDS. 2000 Jul 28;14(11):1545-52. PubMed PMID: 10983641. Epub 2000/09/13. eng.
[54] Vogel M, Friedrich O, Luchters G, Holleczek B, Wasmuth JC, Anadol E, et al. Cancer risk in HIV-infected individuals on HAART is largely attributed to oncogenic infections and state of immunocompetence. Eur J Med Res. 2011 Mar 28;16(3):101-7. PubMed PMID: 21486722. Pubmed Central PMCID: 3352206. Epub 2011/04/14. eng.
[55] Hermine O, Lefrere F, Bronowicki JP, Mariette X, Jondeau K, Eclache-Saudreau V, et al. Regression of splenic lymphoma with villous lymphocytes after treatment of hepatitis C virus infection. N Engl J Med. 2002 Jul 11;347(2):89-94. PubMed PMID: 12110736. Epub 2002/07/12. eng.
[56] Arora R, Shuda M, Guastafierro A, Feng H, Toptan T, Tolstov Y, et al. Survivin is a therapeutic target in Merkel cell carcinoma. Sci Transl Med. 2012 May 9;4(133):133ra56. PubMed PMID: 22572880. Epub 2012/05/11. eng.
 In AMSJ Vol. 3, Issue 2, Michael Li provided an insightful and personal dissertation on the futility of medical treatments and the potential of students to relate to and support patients and their families. [1] Li’s article captures one of the most confronting situations faced by all health professionals, in acknowledging the futility of aiming for a cure, and instead allowing the patient to succumb to their illness. In these situations, clinicians may experience thoughts of frustration, feelings of being powerless, guilt, a sense of professional or personal failure, and an awakened sense of human fragility and mortality. [2] However, the challenges posed by end-of-life decision making across the divergent fields of medicine are not identical. Emergency medicine has long been held as a field of medicine centred upon recognising, treating and stabilising patients with acute illness before they receive definitive care. This is now changing and emergency physicians are experiencing an increasing responsibility for patients with acute, sometimes terminal, exacerbations of chronic, incurable disease. [3,4] Awareness of the values pertinent to end-of-life care, specifically within the emergency department setting, is critical to maintaining patient dignity and preventing unnecessay distress to the patient and their families.
In AMSJ Vol. 3, Issue 2, Michael Li provided an insightful and personal dissertation on the futility of medical treatments and the potential of students to relate to and support patients and their families. [1] Li’s article captures one of the most confronting situations faced by all health professionals, in acknowledging the futility of aiming for a cure, and instead allowing the patient to succumb to their illness. In these situations, clinicians may experience thoughts of frustration, feelings of being powerless, guilt, a sense of professional or personal failure, and an awakened sense of human fragility and mortality. [2] However, the challenges posed by end-of-life decision making across the divergent fields of medicine are not identical. Emergency medicine has long been held as a field of medicine centred upon recognising, treating and stabilising patients with acute illness before they receive definitive care. This is now changing and emergency physicians are experiencing an increasing responsibility for patients with acute, sometimes terminal, exacerbations of chronic, incurable disease. [3,4] Awareness of the values pertinent to end-of-life care, specifically within the emergency department setting, is critical to maintaining patient dignity and preventing unnecessay distress to the patient and their families.