Vulval intraepithelial neoplasia (VIN) is a condition which is increasingly prevalent, particularly in young women, [1] but is a topic rarely touched upon in medical school. The following article reviews current treatment methods for VIN, both surgical and pharmacological, as well as promising new treatment modalities still being researched.
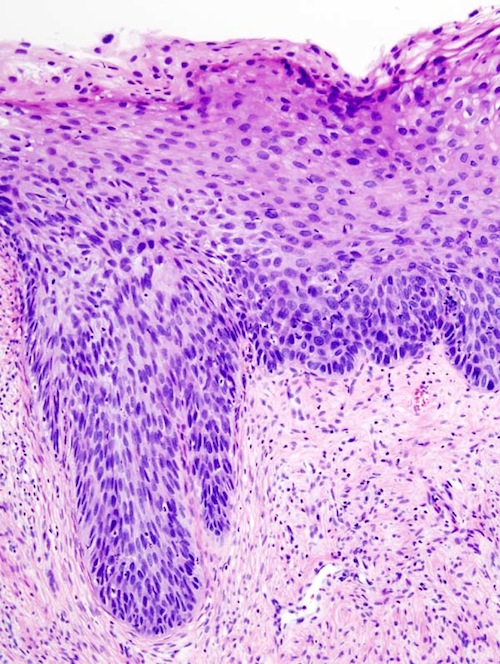
VIN is a condition in which pre-cancerous changes occur in the vulval skin. The incidence of the diagnosis of VIN is approximately 3/100,000, increasing more than four fold since 1973. [2] Vulvar intraepithelial neoplasia is classified into two main groups based on morphologic and histologic features, consisting of VIN usual group and VIN differentiated type. VIN usual group can be subdivided into basaloid and warty subtypes, typically occurs in younger, premenopausal women and is related to HPV infection and cigarette smoking. VIN differentiated type typically occurs in postmenopausal women and is often associated with lichen sclerosus, which presents as white patches on vulval skin. The rate of progression to invasive vulvar cancer in women with untreated high-grade VIN is reported to range from 9.0 to 18.5%. [3] Half of women with VIN are symptomatic, with pruritis, perineal pain or burning, dysuria, a visible lesion or a palpable abnormality. The lesions themselves are often multifocal, raised and can vary in colour from white to red, gray or brown. Diagnosis involves a colposcopic examination, where VIN lesions produce dense acetowhite lesions with or without punctuation. The goals of treatment are prevention of progression to invasive vulvar cancer and symptom relief, as well as preservation of normal vulvar function and anatomy.
Current surgical therapies include excisional treatments or vulvectomy. The main advantage of excisional therapies over ablative or medical treatment is the ability to make a histopathological diagnosis based on the excised lesion, particularly as occult invasive squamous cell carcinoma is present in many of these women. [4]
Wide local excision is the preferred initial intervention for women in whom clinical or pathologic findings suggest invasive cancer, despite a biopsy diagnosis of VIN, to obtain a specimen for pathologic analysis. [4] Localised high-grade VIN lesions are best managed by superficial local excision of an individual lesion, with reported recurrence rates of 20 to 40%. [5]
Multifocal or extensive lesions that are not amenable to removal with local excision are best removed with a partial or simple vulvectomy. This involves removal of part of or the entire vulva, respectively, together with subcutaneous tissue and perineal tissues if indicated; [5] a last resort as neither normal function nor anatomy are preserved.
Laser ablation therapy is an alternative to excisional therapy, particularly for women with multifocal and extensive disease in whom cancer is not suspected. [6] CO2 laser vaporisation has been shown to be effective in eradicating VIN while achieving good cosmetic and functional results, with success rates of 40 to 75%. [6-7]
A systematic review showed that there were no significant differences in recurrence after vulvectomy, partial vulvectomy, local excision or laser evaporisation. [8]
Medical therapies aimed at preserving the vulvar anatomy are useful in younger patients, provided colposcopic examination and biopsies have excluded invasive disease. The primary medical treatment available is Imiquimod 5% cream, which has antiviral and antitumour effects via stimulation of local cytokine production and cell-mediated immunity. [9] A Cochrane review [1] concluded for women with high grade VIN, Imiquimod was better than placebo in terms of reduction in lesion size and histologic regression. This conclusion was based on the findings of three randomised placebo-controlled trials, with the largest trial reporting a complete response rate of 35% and partial response of 46%. [10] Common side effects reported were erythema, soreness, itching, burning, ulceration and flu-like symptoms; however, these side effects were be reduced by placing patients on an escalating dosing regimen. [1]
Agents such as cidofovir, 5-fluorouracil and photodynamic therapy are currently being investigated as treatment for vulval intraepithelial neoplasia. Cidofovir is an acyclic nucleoside analogue with antiviral activity, and a pilot study shows promising results. [11] 5-fluorouracil is a chemotherapeutic agent that inhibits DNA synthesis, with a review demonstrating a remission rate of 34%; [12] however, this agent is used less commonly in current practice. Photodynamic therapy, whereby a sensitizing agent is applied prior to irradiation of the vulva, has been demonstrated to cause complete response in 33 to 55% of patients with VIN 2-3. [7,13]
The major surgical interventions for VIN appear to be similarly effective and are appropriate when there is desire for a histopathological specimen to exclude invasive cancer. Medical interventions are useful when occult cancer is unlikely and preservation of normal vulvar anatomy is desired. Evidence appears to be strongest for Imiquimod as a conservative medical intervention for the treatment of high grade VIN. Other promising agents include cidofovir, but further investigation through large scale studies is required to characterise the efficacy of these therapies. Diligent follow-up is essential in detecting disease recurrence and monitoring the effectiveness of therapies. More research is needed to develop effective treatment strategies that preserve function and anatomy, particularly as the disease becomes more prevalent in young women.
Conflict of interest
None declared.
Correspondence
S Ai: sylvia.ai3@gmail.com
References
[1] Pepas L, Kaushik S, Bryant A, Nordin A, Dickinson HO. Medical interventions for high grade vulval intraepithelial neoplasia. Cochrane Database of Systematic Reviews 2011, Issue 4. Art. No.: CD007924. DOI: 10.1002/14651858.CD007924.pub2.
[2] Judson PL, Habermann EB, Baxter NN, Durham SB, Virnig BA. Trends in the incidence of invasive and in situ vulvar carcinoma. Obstet Gynecol 2006:107(5):1018-22
[3] Joura EA. Epidemiology, diagnosis and treatment of vulvar intraepithelial neoplasia. Gynaecol Oncol Path 2002:14(1):39-43
[4] NSW Department of Health. Best Clinical practice gynaecological cancer guidelines 2009. [online]. Accessed on 28/4/2012 from http://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0010/154549/go_clinical_guidelines.pdf
[5] Holschneider CH. Vulval intraepithelial neoplasia. In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA, 2012.
[6] Hillemanns P, Wang X, Staehle S, Michels W, Dannecker C. Evaluation of different treatment modalities for vulvar intraepithelial neoplasia (VIN): CO2 laser vaporisation, photodynamic therapy, excision and vulvectomy. Gynecol Oncol 2006:100(2):271-5
[7] Sideri M, Spinaci L, Spolti N, Schettino F. Evaluation of CO2 laser excision or vaporisation for the treatment of vulvar intraepithelial neoplasia. Gynecol Oncol 1999:75:277-81.
[8] Van seters, M, van Beurden, M, de Craen, AJM. Is the assumed natural history of vulvar intraepithelial neoplasia III based on enough evidence? A systematic review of 3322 published patients. Gynecol Oncol 2004:97(2):645-51
[9] Mahto M, Nathan M, O’Mahony C. More than a decade on: review of the use of imiquimod in lower anogenital intraepithelial neoplasia. Int J STDs AIDs 2010:21(1):8-16
[10] Van Seters M, van Beurden M, ten Kate FJW, Beckmann I, Ewing PC, Eijkemans MJC et al. Treatment of vulvar intraepithelial neoplasia with topical imiquimod. NEJM 2008:358:1465-73
[11] Tristram A, Fiander A. Clinical responses to cidofovir applied topically to women with high grade vulval intraepithelial neoplasia. Gynecol Oncol 2005:99(3):652
[12] Sillman FH, Sedlis A, Boyce JG. A review of lower genital intraepithelial neoplasia and the use of topical 5-fluorouracil. Obstet Gynecol Survey 1985:40(4):190-220
[13] Fehr MK, Hornung R, Schwarz VA, Haller SU, Wyss P. Photodynamic therapy of vulvar intraepithelial neoplasia III using topically applied 5-aminolevulinic acid. Gynecol Oncol 2001:80(1):62-6